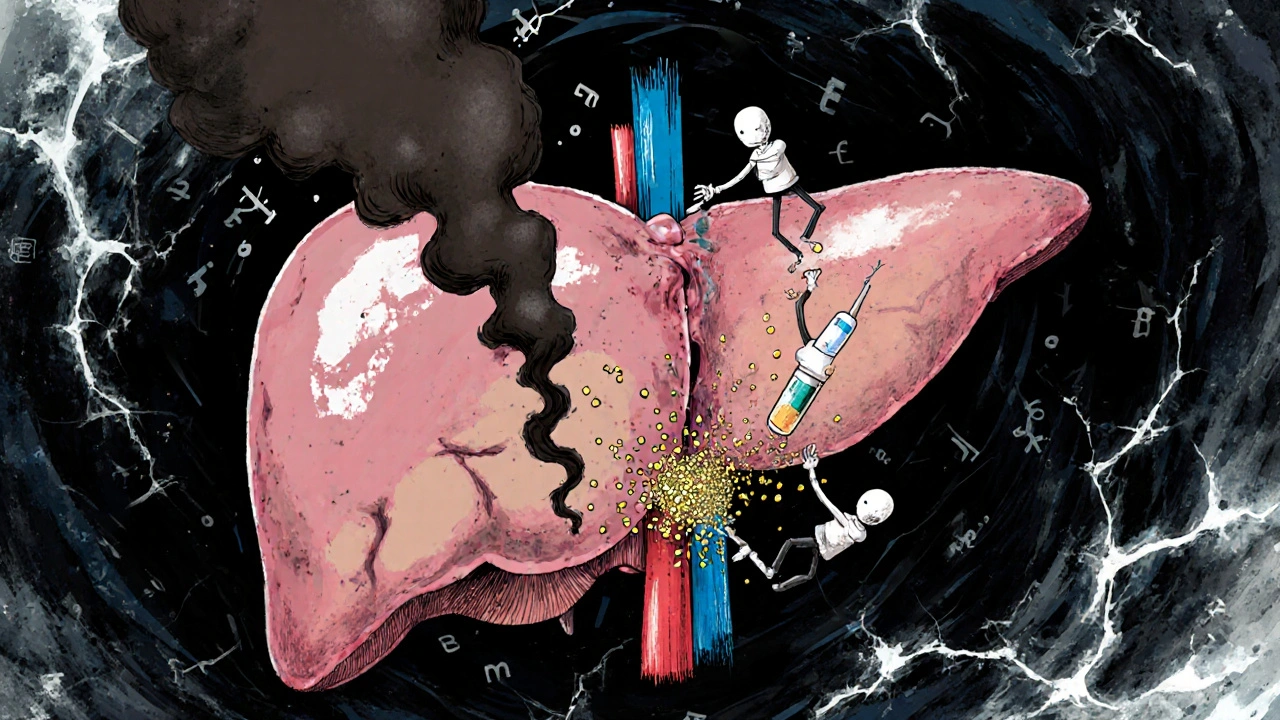
Alcohol and Diabetes Medications: How Alcohol Causes Hypoglycemia and Harms the Liver
 Nov, 26 2025
Nov, 26 2025
Drinking alcohol while taking diabetes medication isn’t just a bad idea-it can be dangerous, even life-threatening. If you’re on insulin, sulfonylureas, or metformin, alcohol doesn’t just affect your hangover. It messes with your blood sugar and your liver in ways you might not notice until it’s too late.
Why Alcohol Drops Your Blood Sugar
Your liver has two big jobs: keeping your blood sugar steady and cleaning out alcohol. When you drink, it drops everything else to deal with the alcohol first. That means it stops releasing glucose into your bloodstream. If you’re taking insulin or a sulfonylurea like glipizide or glyburide, your body is already pushing insulin to lower blood sugar. Add alcohol, and your blood sugar can crash-sometimes hours after your last drink.This isn’t just a theory. People with diabetes report waking up in the middle of the night with shaking, sweating, and confusion, only to find their blood sugar at 45 mg/dL. They didn’t eat after drinking. They didn’t skip a meal. But the alcohol had already shut down their liver’s glucose release. By the time they woke up, it was too late to react.
Here’s the scary part: symptoms of low blood sugar-dizziness, slurred speech, confusion, weakness-look exactly like being drunk. If you pass out after a few drinks, someone might assume you’re just intoxicated. They won’t think to check your blood sugar. And if you have hypoglycemia unawareness, you won’t even feel the warning signs. That’s why so many ER visits for low blood sugar happen after a night out.
Metformin and Alcohol: A Double Hit on the Liver
Metformin is one of the most common diabetes pills. It’s generally safe. But when you add alcohol, things get risky. Both metformin and alcohol are processed by the liver. When they’re together, the liver gets overloaded. This raises your chance of lactic acidosis-a rare but serious condition where lactic acid builds up in your blood. It can cause nausea, vomiting, abdominal pain, and rapid breathing. In severe cases, it leads to organ failure.Even if you don’t develop lactic acidosis, mixing metformin and alcohol makes stomach problems worse. Bloating, cramps, nausea, and diarrhea are common with metformin. Alcohol irritates your gut too. Together, they turn a mild side effect into something unbearable. One patient in Edinburgh told me she stopped drinking entirely after a single night where she vomited for six hours straight-she thought it was food poisoning. Her doctor told her it was metformin + two glasses of wine.
Chronic drinking makes this worse. Long-term alcohol use can lead to fatty liver disease, hepatitis, or even cirrhosis. If your liver is already damaged, metformin becomes harder to process. Your doctor might have to stop the medication altogether. That means tighter blood sugar control becomes much harder.
Which Diabetes Medications Are Riskiest with Alcohol?
Not all diabetes drugs react the same way with alcohol. Here’s the breakdown:- Insulin: Highest risk. Alcohol blocks glucose release from the liver while insulin keeps pushing sugar into cells. A dangerous combo.
- Sulfonylureas (glipizide, glyburide, glimepiride): Also high risk. They force your pancreas to make more insulin. Alcohol makes that insulin work harder than it should.
- Metformin: Moderate risk. Not directly linked to hypoglycemia, but increases liver stress and lactic acidosis risk.
- GLP-1 agonists (semaglutide, liraglutide): Lower risk. These don’t cause low blood sugar on their own, but alcohol can still mask symptoms.
- SGLT2 inhibitors (empagliflozin, dapagliflozin): Be careful. These increase urine sugar output. Alcohol can dehydrate you, raising the risk of ketoacidosis.
If you’re on insulin or a sulfonylurea, you’re in the highest-risk group. Even one drink can trigger a low. There’s no safe amount-only safer choices.
How to Drink Safer (If You Choose To)
The American Diabetes Association doesn’t say “never drink.” They say: Know your risk, and plan ahead. Here’s how:- Never drink on an empty stomach. Eat a meal or snack with carbs before and while drinking. A slice of whole grain bread, a small apple, or a handful of crackers can slow alcohol absorption and give your liver something to work with.
- Choose low-sugar drinks. Avoid sweet cocktails, sugary mixers, and regular soda. Stick to dry wine, light beer, or spirits with soda water and lime. A 5 oz glass of dry white wine has about 1 gram of sugar. A margarita? Up to 20 grams.
- Limit your intake. Stick to one drink per day for women, two for men. That’s one 12 oz beer, 5 oz wine, or 1.5 oz spirits. More than that? You’re increasing liver stress and hypoglycemia risk.
- Check your blood sugar before, during, and after. Test before you start drinking. Test every 1-2 hours while drinking. Test again before bed. If your level is below 100 mg/dL, eat a snack. Don’t wait until you feel symptoms.
- Wear medical ID. If you collapse, someone needs to know you have diabetes-not that you’re just drunk.
- Tell someone. Make sure a friend or family member knows your symptoms of low blood sugar. They might be the only one who notices when you’re too confused to speak clearly.
What About Nighttime Hypoglycemia?
This is the silent killer. Alcohol can cause low blood sugar up to 12 hours after your last drink. That’s why so many people wake up in the middle of the night drenched in sweat, heart racing, terrified.One patient in Glasgow set an alarm for 2 a.m. after drinking. He checked his CGM. His blood sugar had dropped to 58 mg/dL. He ate two glucose tablets. He didn’t wake up again until morning. He’s been doing that every time he drinks since.
Continuous glucose monitors (CGMs) like the Dexcom G7 or FreeStyle Libre 3 help. They show trends. You’ll see your sugar start to fall hours after your last drink. But CGMs don’t detect alcohol-they just show the result. You still need to connect the dots.

What If You’re Not Sure?
Talk to your doctor. Not your pharmacist. Not a Reddit thread. Your doctor. They know your medications, your liver function, your history of lows. They can tell you if your risk is high or low.Here’s what to ask:
- “Is my current medication combo safe with alcohol?”
- “Do I have signs of liver damage?”
- “Should I adjust my dose if I plan to drink?”
- “What should I do if I have a low after drinking?”
A 2021 study found that nearly 6 out of 10 doctors never ask their diabetic patients about alcohol. Don’t wait for them to bring it up. Bring it up yourself.
Bottom Line
Alcohol and diabetes medications don’t mix well. The risk isn’t theoretical. It’s happening every day-in hospitals, in homes, in emergency rooms. If you choose to drink, do it with eyes wide open. Eat first. Test often. Know your limits. Wear your ID. Tell someone.But if you’re unsure? Skip it. There’s no reward worth risking your life.
Can I have one drink if I’m on metformin?
An occasional drink-like one glass of wine with dinner-is usually okay if you eat food and don’t drink on an empty stomach. But metformin and alcohol both stress the liver. If you have any liver issues, drink nothing. Always check with your doctor first.
Why does alcohol cause low blood sugar hours later?
Your liver prioritizes breaking down alcohol over releasing glucose. This effect can last for hours, especially if you’ve been active or didn’t eat. That’s why lows often happen at night or the next morning-long after the alcohol is gone.
Can alcohol make diabetes worse over time?
Yes. Heavy drinking can lead to insulin resistance, fatty liver disease, and pancreas damage. This makes blood sugar harder to control. Over time, it can speed up complications like nerve damage and kidney disease.
Do all diabetes medications react the same with alcohol?
No. Insulin and sulfonylureas carry the highest risk of causing low blood sugar. Metformin doesn’t cause lows directly but increases liver strain. GLP-1 agonists and SGLT2 inhibitors have lower hypoglycemia risk but still need caution due to dehydration and ketoacidosis.
Should I avoid alcohol completely if I have type 2 diabetes?
Not necessarily. Many people with type 2 diabetes drink moderately without issues. But it depends on your meds, your liver health, and your history of low blood sugar. If you’ve had a dangerous low after drinking before, it’s safest to avoid alcohol. Always talk to your doctor.

Tom Shepherd
November 27, 2025 AT 03:29just had a beer after dinner and checked my bg it was 98 so maybe one drink is fine if you eat but holy crap i didnt know alcohol could knock you out hours later
Mira Adam
November 28, 2025 AT 05:37so let me get this straight-your liver is basically a drunk intern who abandons all other duties to deal with the alcohol emergency? and we wonder why people die from this? this isn't medicine, it's a betrayal by your own body
Kaleigh Scroger
November 29, 2025 AT 01:25the most dangerous part isn't the hypoglycemia it's the misdiagnosis. emergency responders see slurred speech and assume intoxication. they don't check glucose. i've seen three patients in the ER over two years who coded because no one thought to test. wear your medical ID. tell someone. it's not optional. your life depends on it
Frances Melendez
November 29, 2025 AT 12:06of course you're telling people to drink 'safely'-because god forbid we ask people to just stop. you're enabling self-destruction with a checklist. if you need a six-step plan to drink alcohol without dying, maybe you shouldn't drink at all. this isn't a lifestyle choice, it's a medical liability
Jonah Thunderbolt
November 29, 2025 AT 21:18alcohol + metformin = liver screaming into a pillow while your pancreas weeps in the corner. 🥲 i used to think i was being 'responsible' with one glass of wine. now i know i was just one bad night away from lactic acidosis. i quit. and honestly? my energy's better. my skin's clearer. my brain doesn't feel like wet cardboard. 🙏
archana das
December 1, 2025 AT 13:38in india we drink mostly wine or beer with dinner. my uncle has type 2 and he drinks one glass every night. he checks his sugar before bed. he eats dal and rice. he never passed out. maybe it's not about never drinking. maybe it's about respecting your body. not fearing it
Aishwarya Sivaraj
December 1, 2025 AT 18:53i was on metformin for three years and drank wine twice a week. never had a low. but then i got fatty liver from stress and my doctor said stop. it wasn't the alcohol alone. it was the combo of stress poor sleep and meds. your liver doesn't care why you're tired. it just knows it's overwhelmed. listen to your body not the internet
Sam HardcastleJIV
December 2, 2025 AT 05:38It is, of course, profoundly regrettable that the medical establishment continues to treat alcohol consumption as a negotiable variable in the management of metabolic disease, rather than as an existential threat to hepatic integrity. One must question the epistemological foundations of public health messaging that permits even 'moderate' ingestion of ethanol in the context of insulin dysregulation.
Elizabeth Choi
December 3, 2025 AT 01:19you say 'one drink' is okay but you don't say what 'one drink' means. is it 5 oz wine? 12 oz beer? 1.5 oz vodka? and what if your CGM is 15 minutes behind? and what if you're on vacation and your snack is a bag of chips? this advice is useless without context. people die because they followed generic advice
reshmi mahi
December 3, 2025 AT 21:48oh wow so now we have to carry a medical ID and tell our friends we're diabetic before we go out? next you'll say we need to wear a sign saying 'don't let me die from bad choices' 🤦♀️ i mean come on india drinks all the time and we don't have this drama
laura lauraa
December 4, 2025 AT 17:35And yet... you still drink. You know the risks. You've read the studies. You've seen the ER reports. You've heard the stories. And still-you pour. Why? Is it the ritual? The escape? The false comfort? Or is it simply that you'd rather die with a glass in your hand than live without it? You're not brave. You're tragic.
Sue Haskett
December 5, 2025 AT 08:13My sister, who's on insulin, once passed out after a single glass of wine. No one knew she had diabetes. She woke up in the ER with a 38. She's been sober for two years now. She says the scariest part wasn't the low-it was realizing how easily she could've died, and how no one would've noticed. Please. Just. Check. Your. Sugar. Before. Bed.