Bioequivalence and Patient Safety: Why Testing Ensures Safe Generic Medications
 Dec, 8 2025
Dec, 8 2025
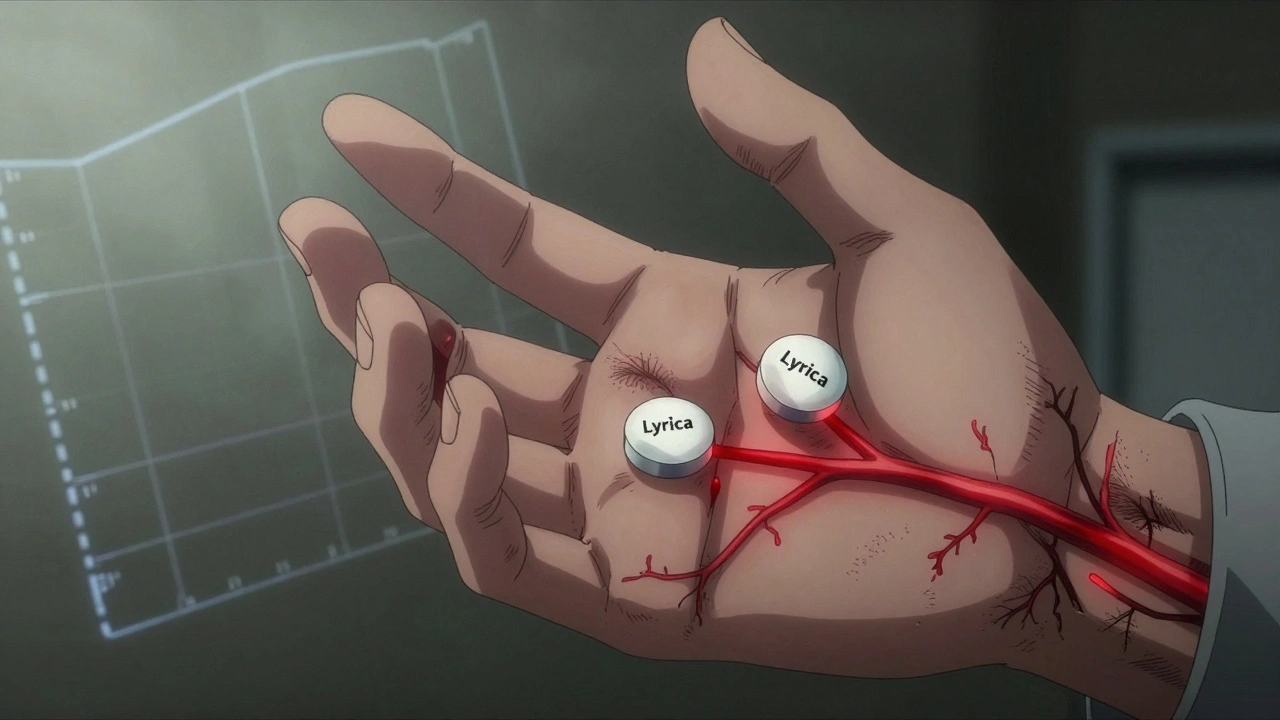
When you pick up a prescription at the pharmacy and see a different name on the bottle - maybe it’s no longer Lyrica but pregabalin - you might wonder: Is this the same thing? Will it work the same? Could it hurt me? These aren’t just random concerns. They’re critical questions tied to something called bioequivalence, and it’s the invisible gatekeeper between affordable medicine and patient safety.
What Bioequivalence Really Means
Bioequivalence isn’t marketing jargon. It’s a precise scientific standard. Two drugs are bioequivalent if they deliver the same amount of active ingredient into your bloodstream at the same rate. That means your body absorbs and uses them in nearly identical ways. The FDA and EMA don’t just assume this - they test it. Every single generic drug must pass these tests before it hits the shelf.The gold standard? Measure how much of the drug shows up in your blood over time. Two numbers matter most: AUC (total exposure) and Cmax (peak concentration). For most drugs, the generic’s values must fall between 80% and 125% of the brand-name drug’s. That’s not a guess. It’s a statistical range based on decades of clinical data. If it’s outside that range, the drug doesn’t get approved.
Why 80-125%? Because small differences are normal. Your body doesn’t absorb every pill the exact same way. Food, gut bacteria, even how fast you swallow can change absorption. The range accounts for that natural variation - but only up to a point. If the difference is bigger, the risk of underdosing or overdosing rises. And that’s where patient safety comes in.
Why This Matters for Your Health
Imagine you’re on warfarin, a blood thinner. Too little, and you risk a clot. Too much, and you could bleed internally. That’s a narrow therapeutic index - a tiny window between effective and dangerous. For these drugs, the acceptable range tightens to 90-111%. Why? Because even a 10% drop in blood levels could trigger a stroke. Bioequivalence testing makes sure that switch from brand to generic doesn’t accidentally put you at risk.Same goes for levothyroxine, used for thyroid disorders. In 2012, the FDA tightened standards after reports of patients having unstable hormone levels after switching generics. They didn’t ban generics - they made the testing stricter. Today, only generics that meet the new, tighter bioequivalence criteria are allowed. That’s patient safety in action.
And it works. A 2022 survey by the National Community Pharmacists Association found 87% of patients reported generics worked just as well as brand names. The FDA’s adverse event database shows generic drugs with confirmed bioequivalence are involved in just 0.07% of reported adverse events - far lower than brand-name drugs at 2.3%. That’s not luck. That’s science.
Not All Drugs Are Created Equal
Bioequivalence testing isn’t one-size-fits-all. For drugs with highly variable absorption - like certain epilepsy meds or statins - regulators use something called scaled average bioequivalence. This lets the acceptable range widen to 75-133%, but only if the drug’s own variability is high. And even then, there’s a catch: the average difference between generic and brand can’t be too large. This prevents a drug that’s wildly inconsistent from slipping through.Then there are complex products - creams, inhalers, eye drops. These aren’t swallowed. They’re applied locally. Measuring blood levels doesn’t tell you if the drug is working where it needs to. That’s why the FDA and EMA now require additional tests: in-vitro performance, skin penetration studies, lung deposition analysis. A generic asthma inhaler might have the same chemical formula, but if the particles don’t reach deep into the lungs like the brand, it’s useless. Bioequivalence testing for these products is evolving fast.
Biosimilars - generic versions of biologic drugs like Humira or Enbrel - are a whole different ballgame. They’re made from living cells, not chemicals. You can’t just copy the formula. You need to prove they behave the same in the body through multiple layers of testing: structural analysis, immune response checks, clinical trials. The bar is higher because the molecules are bigger and more fragile.
How Testing Is Done - And Who Pays
Bioequivalence studies usually happen in healthy volunteers. They take a single dose of the brand or generic drug, then have their blood drawn every 15 to 30 minutes for 24-72 hours. The data is fed into statistical models to see if the curves match. These studies cost $1-2 million each and take 12-18 months. That’s why big pharmaceutical companies don’t do them alone - they hire contract research organizations (CROs) like PPD or WuXi AppTec, which specialize in this kind of testing.But it’s not just about money. Recruiting volunteers who meet strict criteria - healthy, BMI between 18.5 and 30, no liver or kidney issues - is hard. So are studies done with food. Some drugs absorb better with a meal. Others don’t. Regulators require both fasting and fed studies unless it’s unsafe. Japan, for example, only allows fasting studies even if the brand is taken with food - if the drug can still be measured in blood. These differences make global approval complicated.
That’s why groups like the International Pharmaceutical Regulators Programme are pushing for global harmonization. Right now, 134 countries have bioequivalence requirements. In 2015, that number was 89. More countries are catching up - because they know cheap medicine means nothing if it’s unsafe.
What About Patient Stories?
You’ve probably seen posts online: “I switched to generic sertraline and felt awful.” Or “My blood pressure went wild after the pharmacy changed my pill.” These stories are real. And they’re heartbreaking.But here’s what those stories don’t show: the FDA tracks every single adverse event linked to a generic drug. If a pattern emerges - say, 50 people all report the same issue after switching to one specific generic - the agency investigates. They check the manufacturing, the bioequivalence data, the lab results. If the drug failed the test, it gets pulled. In the past five years, only a handful of generics have been recalled for bioequivalence issues.
Most of the time, what patients feel isn’t due to the drug failing bioequivalence. It’s due to placebo effect, changing pill shape or color, or even anxiety about switching. A 2023 Reddit thread about sertraline had 342 comments. Only 37 people reported problems. Pharmacists in the thread pointed out: “The FDA would have flagged this if it were a systemic issue.”
That’s the difference between anecdote and evidence. Bioequivalence testing isn’t perfect. But it’s the best tool we have to prevent harm at scale.

The Bigger Picture: Cost vs. Safety
Generic drugs make up 90% of prescriptions in the U.S. but only 23% of drug spending. In 2020, they saved the healthcare system $313 billion. Without bioequivalence testing, that savings wouldn’t exist. Patients would be stuck paying $500 for a drug that’s chemically identical and available for $10.But here’s the truth: safety isn’t optional. You can’t have cheap medicine that doesn’t work. And you can’t have safe medicine that no one can afford. Bioequivalence is the bridge. It lets you get the same treatment for a fraction of the cost - without risking your health.
Regulators keep improving it. The FDA’s 2023 draft guidance now covers 1,873 specific drugs with tailored testing rules. AI is being tested to predict bioequivalence from dissolution profiles - meaning fewer human studies in the future. But the core principle stays the same: if it doesn’t perform the same in your body, it doesn’t get approved.
What You Can Do
If you’re switching to a generic:- Ask your pharmacist if the generic has been approved under current bioequivalence standards.
- Keep track of how you feel - especially in the first few weeks.
- Don’t assume all generics are the same. Different manufacturers may use different fillers or coatings that affect absorption - even if the active ingredient is identical.
- If you notice changes in effectiveness or side effects, tell your doctor. Don’t ignore it.
Most of the time, you won’t notice a difference. And that’s the point. Bioequivalence testing was designed so you never have to wonder.
Are generic drugs as safe as brand-name drugs?
Yes - if they’ve passed bioequivalence testing. The FDA and EMA require generics to prove they deliver the same amount of active ingredient at the same rate as the brand. Once approved, they’re considered therapeutically equivalent. Adverse event data shows generics with confirmed bioequivalence are involved in far fewer safety issues than brand-name drugs.
Can switching to a generic cause side effects?
It’s rare, but possible. Most side effects after switching are due to changes in inactive ingredients - like dyes or fillers - not the active drug. For narrow therapeutic index drugs like warfarin or levothyroxine, even small changes in absorption can matter. That’s why regulators use tighter limits for these drugs. If you notice new symptoms after switching, talk to your doctor. It’s not always the generic - but it’s worth checking.
How do regulators ensure bioequivalence is accurate?
Regulators require strict study protocols: randomized, crossover designs, precise blood sampling, validated lab methods. The 90% confidence interval for AUC and Cmax must fall within 80-125% (or tighter for some drugs). Independent labs verify results, and manufacturers must submit raw data. The FDA and EMA also audit facilities and review all study reports before approval.
Why do some generics cost more than others?
Cost differences come from manufacturing, branding, and market competition - not bioequivalence. Two generics with the same active ingredient may have different fillers or coatings, which can affect how fast they dissolve. But if both passed bioequivalence testing, they’re equally effective. The higher-priced one isn’t better - it’s just marketed differently.
Is bioequivalence testing the same worldwide?
Most major regulators - FDA, EMA, Health Canada, TGA - follow similar standards. But some countries have unique rules. Japan requires fasting studies even if the brand is taken with food. Brazil mandates more medical screenings than others. The WHO and IPRP are working to align these rules globally, but differences still exist. Always check if a generic is approved by your country’s health authority.
Bioequivalence testing isn’t flashy. It doesn’t make headlines. But every time you fill a prescription and pay less - and stay healthy - it’s because someone ran the numbers, took the blood samples, and made sure the numbers matched. That’s not just science. That’s safety.

Lauren Dare
December 8, 2025 AT 18:44Oh wow, so the FDA just magically knows what my body will do with a pill? I mean, I’ve had generics that made me feel like a zombie and others that made me feel like I’d been injected with espresso. But sure, let’s trust the 80-125% range like it’s some kind of divine oracle. 🙄
Gilbert Lacasandile
December 10, 2025 AT 00:39I think this is actually really well explained. I used to worry about switching generics too, but after reading this, I get how much testing goes into it. It’s not just about the active ingredient - it’s about how your body handles it. Makes sense.
Lola Bchoudi
December 11, 2025 AT 22:00Let’s unpack the bioequivalence framework here - AUC and Cmax aren’t just buzzwords, they’re pharmacokinetic anchors. The 90% CI within 80–125% isn’t arbitrary; it’s derived from population pharmacodynamics and intra-individual variability models. When regulators tighten thresholds for NTIDs like levothyroxine, they’re applying Bayesian risk-benefit analyses rooted in real-world outcomes. This isn’t bureaucracy - it’s precision medicine in action.
Morgan Tait
December 13, 2025 AT 11:08Did you know the FDA gets paid by pharma to approve these generics? I mean, think about it - why would they risk patient safety? They’re in bed with the big drug companies. And those CROs? WuXi AppTec? They’ve got ties to China. What if the blood samples get swapped? Or the lab results are faked? I’ve seen the footage - the volunteers are all paid addicts. They don’t even know what they’re taking. This isn’t science. It’s a cover-up.
Darcie Streeter-Oxland
December 13, 2025 AT 18:56While the content presented is undoubtedly comprehensive and grounded in empirical regulatory frameworks, one cannot help but observe a conspicuous absence of critical discourse regarding the potential for systemic bias in the selection of healthy volunteer cohorts. The generalizability of pharmacokinetic data derived from a narrow demographic (BMI 18.5–30, no comorbidities) to the broader, polypharmacological elderly population remains, in my estimation, inadequately substantiated.
Taya Rtichsheva
December 15, 2025 AT 15:53Mona Schmidt
December 16, 2025 AT 21:25It’s important to remember that bioequivalence doesn’t mean identical - it means therapeutically equivalent. The fillers, coatings, and dissolution profiles can differ, and that’s why some people notice changes. But that doesn’t mean the drug is unsafe. It means we need better patient education. Talk to your pharmacist. Ask about the manufacturer. Track your symptoms. Knowledge is power - and safety.
Guylaine Lapointe
December 18, 2025 AT 13:45Oh please. If generics were truly safe, why do so many people report side effects after switching? The FDA’s database is full of holes. They only count what’s reported, and most people don’t bother. And don’t give me that ‘placebo effect’ nonsense - if my anxiety spiked and my heart started racing after a pill change, it’s not in my head. It’s in the pill. And someone’s profit margin is the reason we’re being told to shut up and take it.
Kathy Haverly
December 19, 2025 AT 09:57Let’s be real - this whole bioequivalence thing is a corporate smokescreen. The 80–125% range? That’s a 45% swing. That’s not equivalence - that’s a gamble. And the fact that they test on healthy 22-year-olds while old people with kidney failure take these drugs? That’s not science. That’s criminal negligence. And don’t even get me started on how they ignore drug interactions. You think your 70-year-old grandma on 8 meds is getting a safe generic? Wake up.
Andrea DeWinter
December 20, 2025 AT 23:04Steve Sullivan
December 21, 2025 AT 01:28Bro. I just want to say… 🤔❤️🩹 this post made me cry a little. Not because I’m emotional - but because I realized how much invisible labor goes into making sure my $4 pill doesn’t kill me. The scientists. The volunteers. The regulators. The pharmacists. We take this for granted. And now I’m gonna thank my pharmacist tomorrow. Also… can we make a meme? ‘Bioequivalence: The Quiet Hero of Your Medicine Cabinet’? 🙏💊
George Taylor
December 21, 2025 AT 14:12Yet… despite the statistically significant data, the anecdotal evidence persists - and is dismissed as ‘placebo’ or ‘anxiety.’ This is a classic case of confirmation bias masked as scientific rigor. The FDA’s adverse event reporting system is notoriously underutilized - and when a pattern emerges, the response is often delayed, obfuscated, or attributed to ‘individual variability.’ The data is clean - but the system is not.
Chris Marel
December 23, 2025 AT 01:09This is really helpful. I’m from Nigeria, and we don’t always have access to brand-name meds. Knowing that there’s a science behind generics gives me peace. But I do worry - sometimes the generics here aren’t even approved by our own agency. Maybe this kind of info should be shared more in places like mine.
Evelyn Pastrana
December 24, 2025 AT 07:44So… basically, your generic pill is like a cousin of the brand name. Same DNA, different haircut. Sometimes you don’t notice. Sometimes it’s weird. But unless it’s warfarin or thyroid meds, you’re probably fine. And hey - you saved $40. That’s a win. 🙌
Steve Sullivan
December 25, 2025 AT 06:47Love this. I’ve been thinking about this since I read your comment. What if we started a community wiki? Like, ‘Which generics work best for [med]?’ with real user reports + manufacturer names? Could save people from bad batches. 🤝