Biologics in Severe Asthma: How Anti-IgE and Anti-IL-5 Therapies Work
 Jan, 21 2026
Jan, 21 2026
When Inhalers Aren’t Enough
For most people with asthma, inhalers work well. But for those with severe asthma, even high-dose steroids and long-acting bronchodilators don’t stop the coughing, wheezing, or midnight panic attacks. These patients keep ending up in emergency rooms, relying on oral steroids that wreck their bones, blood sugar, and mood. That’s where biologics come in-not as magic pills, but as precision tools that target the exact immune signals driving their asthma.
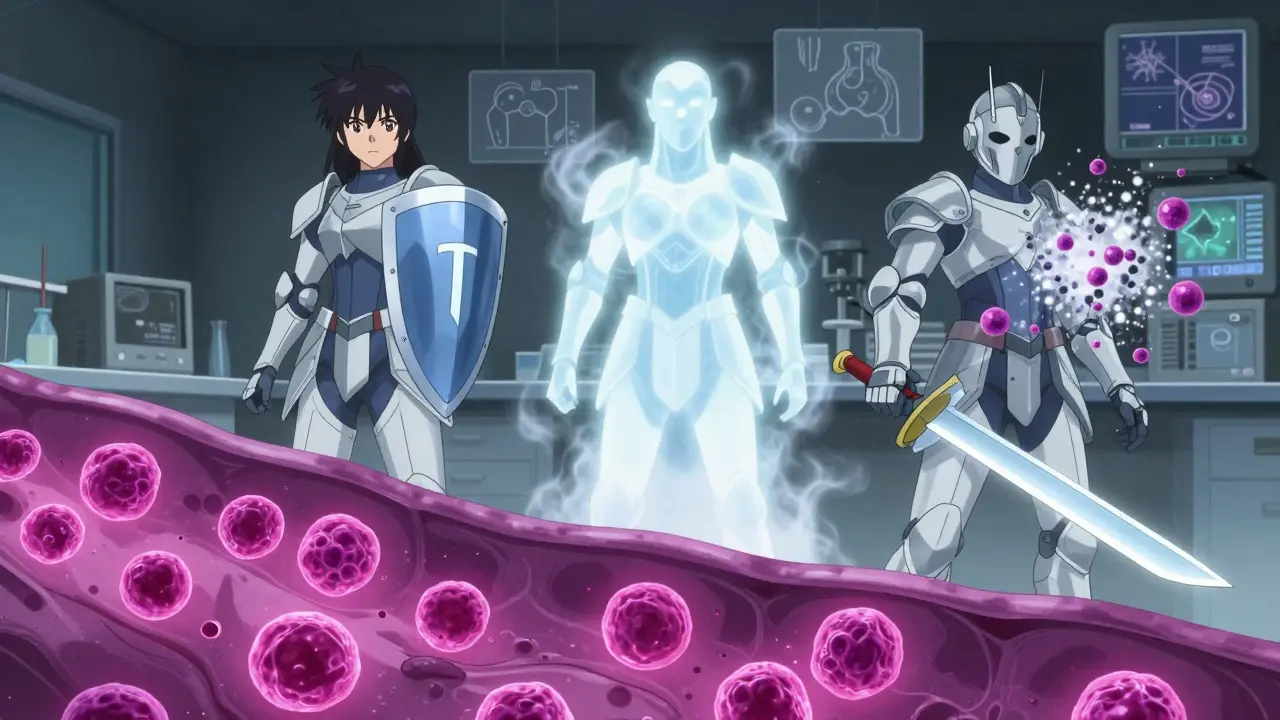
Unlike traditional drugs that broadly suppress inflammation, biologics are made from living cells and act like guided missiles. They zero in on one specific molecule in the immune system. Two of the most established types are anti-IgE and anti-IL-5 therapies. They don’t cure asthma, but for the right people, they cut flare-ups in half and let many stop oral steroids for good.
What Is Anti-IgE Therapy?
Anti-IgE therapy starts with IgE-the antibody that triggers allergic reactions. In allergic asthma, your body overreacts to things like dust mites, pet dander, or mold. IgE binds to mast cells and basophils, which then blast out histamine and other chemicals that cause airway swelling and mucus. Omalizumab (brand name Xolair) blocks IgE before it can activate these cells. No IgE binding = no allergic cascade.
This therapy is only for people with clear allergic asthma. You need to test positive for at least one perennial allergen (like house dust mites or cockroaches), and your total IgE blood level must be between 30 and 1500 IU/mL. It’s not for non-allergic asthma or sudden flare-ups. Omalizumab doesn’t work fast-it takes weeks to months to show results. But once it does, patients often report fewer ER visits and less reliance on prednisone.
Dosing is based on your weight and IgE level. Most people get a shot every 2 to 4 weeks. It’s self-administered with an auto-injector pen after training. Side effects? Mostly mild: soreness at the injection site, headache, or sore throat. A rare but serious risk is anaphylaxis-about 1 in 1,000 doses. That’s why the first few injections are given in a clinic.
How Anti-IL-5 Therapies Target Eosinophils
Not all severe asthma is allergic. Many patients have high levels of eosinophils-white blood cells that cause airway inflammation. This is called eosinophilic asthma. Anti-IL-5 drugs stop these cells from forming, surviving, or attacking the lungs.
There are three main ones: mepolizumab (Nucala), reslizumab (Cinqair), and benralizumab (Fasenra). All target interleukin-5 (IL-5), a protein that tells eosinophils to multiply. But they work differently.
Mepolizumab and reslizumab latch onto IL-5 itself, preventing it from reaching eosinophils. Reslizumab is given as an IV infusion every 4 weeks, so you need to go to a clinic. Mepolizumab is a shot you can give yourself at home every 4 weeks. Benralizumab goes a step further-it binds directly to the IL-5 receptor on eosinophils and triggers the immune system to kill those cells. This means eosinophil counts can drop by 95% within 24 hours.
To qualify, your blood eosinophil count must be at least 150 cells/μL in the past year, or 300 cells/μL if you’ve had recent flare-ups. These drugs are most effective in people with high eosinophils, even if they’re not allergic. In clinical trials, they reduced asthma attacks by 50% or more. One patient in Edinburgh told me she went from 4 hospitalizations a year to zero after 6 months on mepolizumab.
Comparing Anti-IgE and Anti-IL-5
Choosing between anti-IgE and anti-IL-5 isn’t about which is ‘better.’ It’s about which matches your asthma type.
| Feature | Anti-IgE (Omalizumab) | Anti-IL-5 (Mepolizumab, Benralizumab, Reslizumab) |
|---|---|---|
| Target | Immunoglobulin E (IgE) | Interleukin-5 (IL-5) or its receptor |
| Best for | Allergic asthma with positive allergen tests | Eosinophilic asthma, regardless of allergy status |
| Biomarker needed | Serum IgE level (30-1500 IU/mL) | Blood eosinophil count ≥150-300 cells/μL |
| Typical dosing | Every 2-4 weeks, subcutaneous | Every 4 weeks (mepolizumab, reslizumab); every 8 weeks after initial doses (benralizumab) |
| Administration | Self-injection | Self-injection (omalizumab, mepolizumab, benralizumab); IV infusion (reslizumab) |
| Onset of effect | 3-6 months | 2-4 months (benralizumab may act faster) |
| Reduction in exacerbations | ~50% | 51-52% |
| Oral steroid reduction | Up to 50% | Up to 60% |
Benralizumab stands out because it doesn’t just block IL-5-it kills eosinophils. That’s why some patients see results faster. But it’s not for everyone. One Reddit user reported severe joint pain after three doses and had to stop. Side effects vary. Injection site reactions happen in up to 30% of people at first, but often fade after a few shots.
Who Gets These Treatments?
These aren’t first-line drugs. Before even considering a biologic, your doctor must confirm you’re doing everything right with standard care: proper inhaler technique, consistent use, avoiding triggers, and managing reflux or sinus issues. Many patients think they’re on ‘maximum therapy’-but they’re not using their inhalers correctly.
Guidelines from the European Respiratory Society and GINA say biologics are only for those who still have uncontrolled asthma despite using medium-to-high dose inhaled corticosteroids plus long-acting beta agonists. You need a history of frequent exacerbations-two or more per year requiring oral steroids or hospital visits.
Testing is key. You’ll need blood tests for eosinophils, IgE levels, and sometimes fractional exhaled nitric oxide (FeNO), which measures airway inflammation. Without these, you’re guessing. And guesswork leads to wasted time, money, and frustration. Real-world data shows 30-40% of patients don’t respond to biologics-not because they’re broken, but because they weren’t the right match.
Cost, Access, and Real-World Challenges
These drugs cost $25,000 to $40,000 per year. In the UK, NHS access is limited. Most patients get them through specialist asthma clinics after strict approval. Insurance authorization can take 2-3 weeks. Some patients wait months just to start.
Manufacturers offer co-pay assistance and nurse support lines, which help. But many still drop out because of the cost, the injections, or because they don’t see quick results. Improvement isn’t instant. Some feel better in 4 weeks. Others need 12-16 weeks. If you stop after 3 months because it’s ‘not working,’ you might be giving up too soon.
And it’s not just about asthma control. For many, it’s about freedom. One woman in Glasgow stopped carrying her emergency steroid pack. Another stopped missing work. A teenager who couldn’t run in PE now plays rugby. That’s the real win.

What’s Next?
The field is moving fast. Tezepelumab (Tezspire), approved in 2021, targets TSLP-an upstream trigger that kicks off multiple inflammatory pathways. It works even if your eosinophils are low. That’s huge. It opens the door for more people to benefit.
Researchers are testing twice-yearly injections. One trial is comparing all five major biologics head-to-head in 1,200 patients. Results are due in mid-2025. That could finally tell us which drug works best for which profile.
But the biggest barrier isn’t science-it’s access. Only 1-2% of eligible patients get biologics. Why? Cost, complexity, lack of specialist centers, and low awareness among GPs. In North America, usage is higher. In Asia, it’s barely 0.7%. The goal for the next decade is to make these therapies simpler, cheaper, and available to everyone who needs them.
Is It Worth It?
For the right person, yes. If you’ve been stuck in the cycle of flare-ups, steroids, and ER visits, biologics can change your life. But they’re not for everyone. You need the right asthma type, the right biomarkers, and the right support system.
They don’t replace inhalers. They don’t cure asthma. But they give you back control. And for many, that’s everything.
How long does it take for anti-IgE or anti-IL-5 biologics to work?
Most patients start noticing improvements in 4 to 12 weeks, but full benefits often take 3 to 6 months. Some report fewer nighttime symptoms or less rescue inhaler use earlier. If you don’t see changes after 6 months, your doctor may reassess whether this biologic is right for you.
Can I stop my inhalers if I start a biologic?
No. Biologics are add-on therapies. You must keep using your inhaled corticosteroids and long-acting bronchodilators unless your specialist tells you otherwise. Stopping them can lead to dangerous flare-ups. Biologics reduce inflammation over time, but they don’t replace quick-relief or daily controller meds.
Do these biologics cause weight gain or mood changes?
Unlike oral steroids, biologics don’t cause weight gain, mood swings, or diabetes. Their side effects are mostly local: injection site redness, swelling, or itching. Rarely, patients report headaches or fatigue. Serious allergic reactions are very uncommon. If you’ve had bad reactions to steroids, biologics may be a safer long-term option.
Are biologics safe for children?
Yes. Omalizumab is approved for children as young as 6 with allergic asthma. Mepolizumab and benralizumab are approved for ages 12 and up. Studies show they reduce exacerbations and steroid use in pediatric patients, improving school attendance and activity levels. Pediatric asthma specialists carefully monitor growth and immune response.
What if I miss a dose?
If you miss one dose, take it as soon as you remember. If it’s close to your next scheduled dose, skip the missed one and go back to your regular schedule. Don’t double up. Missing occasional doses usually doesn’t cause immediate problems, but consistent dosing is key for long-term control. Talk to your nurse or specialist if you’re struggling to keep up.
Can I get these biologics through the NHS in the UK?
Yes, but access is limited. The NHS provides biologics only through specialist asthma centers for patients with confirmed severe, uncontrolled asthma despite optimal standard therapy. You’ll need documented exacerbations, biomarker results (eosinophils or IgE), and proof of adherence. Approval can take weeks, and not all eligible patients receive treatment due to budget constraints.
Do biologics work for non-eosinophilic asthma?
Anti-IL-5 drugs (mepolizumab, benralizumab) are designed for eosinophilic asthma and won’t help if your eosinophil count is low. Omalizumab helps only if your asthma is allergic. But tezepelumab (Tezspire), approved in 2021, works across multiple asthma types-even if eosinophils are normal-because it blocks TSLP, an early trigger. This makes it the first biologic that might help a broader group.
Next Steps
If you think you might be a candidate, talk to your asthma specialist. Ask for a review of your asthma control using the Asthma Control Test. Request blood tests for eosinophils and IgE. Bring a log of your flare-ups over the past year. If you’re on oral steroids, ask if you’re eligible for a biologic trial. Don’t assume you’re not a candidate-many people are overlooked because their asthma is labeled ‘difficult to treat’ instead of ‘biologic-responsive.’
These therapies aren’t perfect. But for the right person, they’re not just medicine-they’re freedom.
