How COVID-19 Changed Embolism Risk and What Doctors Are Doing About It
 Oct, 7 2025
Oct, 7 2025
COVID-19 Embolism Risk Calculator
Your Risk Factors
Select any factors that apply to you:
Vaccination Status
Please select your current vaccination status:
Symptom Checker
Check any symptoms you've experienced recently:
Risk Assessment Result
Recommendation:
Quick Takeaways
- COVID-19 spikes clot‑forming proteins, making patients up to three times more likely to develop deep‑vein or pulmonary emboli.
- Severe cases show a distinct "coagulopathy" driven by inflammation and endothelial injury.
- Standard thromboprophylaxis (low‑dose heparin) is often insufficient for ICU patients; higher‑dose regimens are now recommended.
- Biomarkers like D‑dimer and fibrinogen guide real‑time adjustments to anticoagulant therapy.
- Vaccination lowers the overall embolism burden by preventing severe COVID‑19, but long‑COVID can still keep clot risk elevated for months.
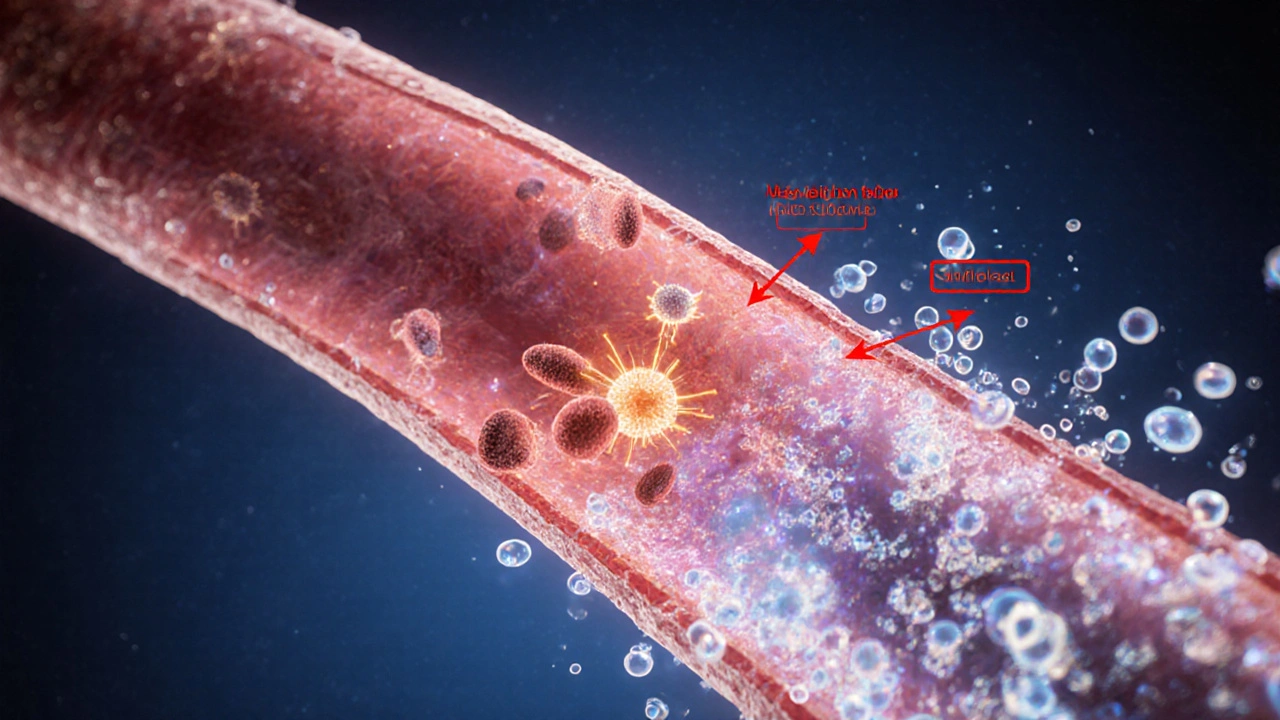
Why COVID‑19 Ramps Up Clot Risk
When COVID-19 is a respiratory virus caused by SARS‑CoV‑2 that triggers a systemic inflammatory response becomes more than a lung infection. The viral spike protein activates the endothelium, the thin lining of blood vessels, causing it to release tissue factor and vonvon Willebrand factor. This endothelial dysfunction turns the vascular system into a pro‑clotting factory.
Two mechanisms dominate:
- Cytokine storm - massive release of interleukin‑6, tumor necrosis factor‑α, and other cytokines ramps up the clotting cascade.
- Direct viral injury - the virus invades endothelial cells, exposing sub‑endothelial collagen that attracts platelets.
Studies from 2022‑2024 show hospitalised COVID‑19 patients have a 2‑3× higher incidence of venous thrombo‑embolism (VTE) compared with non‑COVID patients, even after adjusting for immobilisation and comorbidities.
What Types of Embolism Are Most Common?
Clinicians usually classify embolic events into two buckets:
- Deep‑vein thrombosis (DVT) a clot that forms in the deep veins of the legs or pelvis. In COVID‑19, DVTs often appear in the popliteal or femoral veins within the first week of ICU admission.
- Pulmonary embolism (PE) a clot that breaks off and travels to block arteries in the lungs. PE rates jumped from ~5% in pre‑pandemic ARDS to 15‑20% in severe COVID‑19 ARDS.
Arterial emboli (stroke, limb ischemia) also increase, but they are less frequent than venous events. The shared denominator is a hyper‑coagulable state that short‑circuits the body’s natural anticoagulant pathways.

How Doctors Measure the Clotting Surge
Two laboratory markers dominate risk stratification:
- D‑dimer a fibrin degradation product that rises when clots are broken down. Levels above 2µg/mL on admission predict VTE with >80% sensitivity.
- Fibrinogen - values >600mg/dL correlate with severe inflammation and a higher likelihood of progression from DVT to PE.
Clinicians combine these labs with clinical scores such as the Caprini or IMPROVE risk tools, tweaking the thresholds for COVID‑19 patients. For example, a Caprini score of 5 (moderate risk) may prompt full‑dose anticoagulation in a COVID‑19 ICU setting, whereas the same score would usually warrant only prophylaxis.
Anticoagulant Strategies in the Pandemic Era
The backbone of embolism prevention remains anticoagulation, but the pandemic forced a rapid re‑evaluation of dosing and drug choice. Below is a side‑by‑side look at the three main agents used in hospitalised COVID‑19 patients.
| Agent | Typical Dose (COVID‑19) | On‑set of Action | Renal Considerations | Key Advantage |
|---|---|---|---|---|
| Unfractionated Heparin (UFH) | 10,000U bolus then 1,000U/h (adjust to aPTT 1.5‑2×) | Minutes | Safe in severe renal failure | Rapid reversal with protamine |
| Low‑Molecular‑Weight Heparin (LMWH) - enoxaparin | 1mg/kg twice daily (full dose) or 40mg daily (prophylaxis) | Hours | Dose‑adjust if CrCl <30mL/min | Predictable pharmacokinetics, outpatient use |
| Direct Oral Anticoagulants (DOACs) - apixaban | 5mg BID (full) or 2.5mg BID (prophylaxis) | Hours | Avoid if CrCl <15mL/min | No routine monitoring, easy discharge |
Guidelines from the American Society of Hematology (2023) suggest:
- Standard prophylactic LMWH for non‑ICU patients with mild‑moderate disease.
- Intermediate or therapeutic‑dose anticoagulation for ICU patients with D‑dimer >2µg/mL or documented thrombus.
- Switch to a DOAC once the patient is stable, off ventilator, and has normal renal function.
These recommendations are flexible; clinicians still tailor therapy based on bleeding risk, platelet count, and individual comorbidities.
Balancing Bleeding Risks
Higher anticoagulant doses cut clot rates but increase major bleeding about 2‑fold. Strategies to keep bleeding in check include:
- Daily platelet checks - pause UFH if platelets <50×10⁹/L.
- Watch for gastrointestinal bleeding - consider proton‑pump inhibitor prophylaxis.
- Use viscoelastic testing (TEG/ROTEM) in the ICU to fine‑tune dosing.
Patients with concurrent antiplatelet therapy (e.g., post‑PCI) need a multidisciplinary review to avoid over‑anticoagulation.

Long‑COVID and Ongoing Embolism Risk
Even after the acute infection resolves, a subset of patients-often called "long‑COVID" sufferers-maintain elevated inflammatory markers for weeks to months. A 2024 cohort study of 1,200 post‑COVID patients showed a persistent 1.8× higher incidence of DVT up to six months post‑infection.
Key follow‑up steps:
- Re‑check D‑dimer at 4‑ and 12‑week intervals if it remained >2µg/mL during admission.
- Consider extended prophylaxis with a DOAC for up to 45days in high‑risk individuals (age >65, obesity, prior VTE).
- Encourage graduated physical activity and compression stockings for those with lingering immobilisation.
Vaccination has a clear protective effect: fully vaccinated individuals hospitalized with COVID‑19 exhibit a 30% lower VTE rate compared with unvaccinated peers, likely because the disease course is milder.
Future Directions and Research Gaps
Several unanswered questions still shape research budgets:
- Do viral variants (e.g., Omicron sub‑lineages) differ in their thrombogenic potential?
- Can early anti‑inflammatory therapy (e.g., IL‑6 blockers) blunt the coagulopathy enough to skip therapeutic anticoagulation?
- What is the optimal duration of post‑discharge anticoagulation for patients with only moderately elevated D‑dimer?
Large multinational registries launched in 2025 aim to answer these by pooling real‑world data from over 200 hospitals.
Frequently Asked Questions
Why does COVID‑19 cause more blood clots than other viral infections?
COVID‑19 triggers a unique combination of endothelial injury, massive cytokine release, and direct viral interaction with the clotting cascade. This triple hit overwhelms the body’s natural anticoagulant mechanisms, leading to a higher incidence of deep‑vein and pulmonary emboli compared with flu or other coronaviruses.
Should I be on blood thinners if I test positive for COVID‑19 but stay at home?
For most mild, non‑hospitalised cases, routine anticoagulation isn’t recommended. Instead, stay mobile, hydrate, and watch for leg swelling or shortness of breath. If you have a prior history of thrombosis or significant risk factors (obesity, cancer, recent surgery), talk to your doctor about a short prophylactic course.
How long does the increased clot risk last after recovery?
Studies suggest the heightened risk can linger for 3‑6months, especially if D‑dimer stayed elevated during the acute phase. Follow‑up labs and, in some cases, a 4‑ to 6‑week course of a low‑dose DOAC can reduce late events.
Are the newer COVID‑19 variants less likely to cause clots?
Preliminary data from 2025 indicate that Omicron‑derived sub‑variants still provoke significant coagulopathy in severe cases, though overall hospitalization rates-and thus clot rates-have dropped thanks to widespread immunity.
What symptoms should prompt an immediate call to the doctor?
Sudden leg pain or swelling, unexplained shortness of breath, chest pain that worsens with deep breaths, or a rapid heartbeat are red flags for DVT or PE and require urgent evaluation.

liza kemala dewi
October 7, 2025 AT 17:13The interplay between viral inflammation and coagulation pathways illustrates how a respiratory infection can become a systemic threat.
When SARS‑CoV‑2 engages the endothelial lining, it triggers a cascade that ultimately tips the hemostatic balance toward thrombosis.
This process is not merely a by‑product of immobility; rather, it reflects a profound dysregulation of innate immunity.
Elevated cytokines such as interleukin‑6 act as conductors, orchestrating platelet activation and fibrin formation.
Simultaneously, the virus’s direct invasion of endothelial cells exposes collagen, a potent catalyst for clot initiation.
Consequently, patients with severe COVID‑19 exhibit markedly higher D‑dimer levels, a laboratory hallmark of ongoing fibrinolysis.
Clinicians have therefore adopted intensified anticoagulation protocols, recognizing that standard prophylaxis may be insufficient.
Yet the decision to escalate dosing must be tempered by individual bleeding risk, a nuance that underscores the art of medicine.
Moreover, the persistent hypercoagulable state observed in long‑COVID suggests that the vascular sequelae can outlast respiratory symptoms.
Follow‑up studies indicate that D‑dimer may remain elevated for months, warranting periodic reassessment.
From a public health perspective, vaccination emerges as a critical tool, not only to prevent infection but also to attenuate the severity of coagulopathy.
By reducing the incidence of severe disease, vaccines indirectly diminish the burden of embolic complications.
Nevertheless, clinicians must remain vigilant for clotting events even among vaccinated individuals, as breakthrough infections can still trigger inflammation.
Patient education should therefore emphasize mobility, hydration, and awareness of limb swelling or unexplained dyspnea.
In sum, the pandemic has reshaped our understanding of thrombosis, compelling a more proactive, individualized approach to anticoagulation.
Jay Jonas
October 8, 2025 AT 07:06Man, the way COVID turns your blood into a sticky mess is wild.
I swear the cytokine storm felt like a drama series climax, complete with plot twists.
Bottom line: stay active and keep an eye on any weird leg pain.
Liam Warren
October 8, 2025 AT 11:16From a clinical standpoint, incorporating a high‑intensity LMWH regimen can curtail thrombin generation in ICU cohorts.
Pair that with serial D‑dimer monitoring, and you’ve got a dynamic feedback loop to tailor therapy.
Brian Koehler
October 8, 2025 AT 15:26Indeed, the mechanistic insight into endothelial activation, platelet aggregation, and fibrin cross‑linking underscores the necessity for a calibrated anticoagulation strategy; moreover, individualized risk stratification remains paramount; consequently, multidisciplinary collaboration is essential.
Dominique Lemieux
October 9, 2025 AT 08:06While many herald the pandemic as the catalyst for a revolution in thrombosis management, one must consider that over‑aggressive anticoagulation carries its own perils, including hemorrhagic complications that are often under‑reported.
The literature, albeit robust, is riddled with heterogenous endpoints, making universal protocols precarious.
Furthermore, the emphasis on D‑dimer thresholds may obscure the nuanced interplay of other coagulation factors such as factor VIII and von Willebrand factor.
In my view, a balanced approach that weighs both thrombotic and bleeding risks will ultimately serve patients better than a one‑size‑fits‑all mantra.
Hence, continue to question sweeping guidelines and tailor therapy to the individual clinical tapestry.
Laura MacEachern
October 9, 2025 AT 12:16Absolutely, encouraging gentle leg exercises and regular ambulation can dramatically reduce venous stasis.
Keep hydrated and consider compression stockings if prolonged bed rest is unavoidable.
BJ Anderson
October 10, 2025 AT 03:33The data clearly show a tripling of PE incidence in severe cases; ignoring this trend would be negligent.
Adjust dosing protocols accordingly to safeguard high‑risk cohorts.
Alexander Rodriguez
October 10, 2025 AT 07:43Higher anticoagulation doses have saved lives.
Abhinav Sharma
October 10, 2025 AT 23:00From a mechanistic perspective, the cytokine surge acts as a catalyst that accelerates the coagulation cascade 🙂.
Precise quantification of biomarkers like D‑dimer enables clinicians to stratify risk with greater fidelity 📊.
Therefore, integrating both laboratory data and clinical observation yields the most robust management plan.
Welcher Saltsman
October 11, 2025 AT 03:10Don't overthink it just keep moving and drink water it'll help a lot
april wang
October 11, 2025 AT 18:26When guiding patients through post‑COVID recovery, it is vital to adopt a holistic mindset.
First, assess baseline functional status and identify any residual dyspnea or fatigue.
Second, encourage incremental increases in physical activity, such as short walks progressing to moderate aerobic exercise.
Third, stress the importance of adequate hydration, as plasma volume influences coagulation dynamics.
Fourth, monitor laboratory markers periodically, especially D‑dimer, to detect any lingering hypercoagulable state.
Fifth, educate patients on warning signs like unilateral leg swelling, chest discomfort, or unexplained tachycardia.
Sixth, collaborate with multidisciplinary teams, including physical therapists and hematologists, when complex cases arise.
Seventh, recognize that mental health plays a role; anxiety can exacerbate perceived symptom severity.
Eighth, tailor anticoagulation duration based on individual risk profiles rather than employing blanket protocols.
Ninth, reinforce vaccination as a preventive measure to mitigate severe disease and its thrombotic complications.
Tenth, document all interventions meticulously to facilitate continuity of care.
Finally, maintain open communication channels so patients feel supported throughout their recovery journey.
Vishnu Raghunath
October 11, 2025 AT 22:36Feels like the virus is auditioning for a thriller.
Aparna Dheep
October 12, 2025 AT 16:40One could argue that the clotting cascade is the body's misguided attempt at self‑preservation, a paradox of defense turning destructive.
Yet we tend to overlook how lifestyle factors interplay with viral pathology, creating a perfect storm.
In light of this, personal responsibility cannot be dismissed.
Nicole Powell
October 12, 2025 AT 20:50The article oversimplifies the risk; not every COVID survivor needs anticoagulation.
Clinical decisions must be grounded in evidence, not hype.
Ananthu Selvan
October 13, 2025 AT 14:53Stop glorifying the vaccine as a miracle cure for clotting-it's just one piece of the puzzle.
Overprescribing anticoagulants will drown patients in bleed risk.
Critical thinking is sorely missing in most discussions.
Nicole Chabot
October 13, 2025 AT 19:03Thanks for breaking down the biomarkers; I feel more equipped to discuss my lab results with my doctor.
Any tips on how to stay active while working from home?
Sandra Maurais
October 14, 2025 AT 15:53The statistical analysis presented lacks stratification by age and comorbidity, thus limiting its external validity 📉.
Moreover, the confidence intervals reported are unusually narrow, suggesting potential overfitting 📐.
A more rigorous multivariate model would bolster the credibility of the findings 🧠.
Until such adjustments are made, the conclusions remain provisional.
Michelle Adamick
October 14, 2025 AT 20:03Leverage high‑intensity interval training (HIIT) to boost peripheral circulation and reduce venous stasis 🚀.
Combine this with targeted compression therapy to further mitigate DVT risk 🩺.
Together, these strategies create a synergistic effect that outperforms passive rest.
Edward Glasscote
October 15, 2025 AT 14:06Overall, the post highlights important changes in clot risk post‑COVID.
Staying informed and proactive is the best defense.