How Fatty Foods Boost Absorption of Lipid-Based Medications
 Jan, 12 2026
Jan, 12 2026
When you take a pill with a fatty meal, you’re not just eating-you’re helping your body absorb medicine more effectively. This isn’t just an old wives’ tale. It’s science. For certain medications, especially those designed to treat chronic conditions like high cholesterol, organ transplant rejection, or fungal infections, eating fat isn’t optional-it’s part of the treatment plan.
Why Fat Makes Some Medicines Work Better
Not all drugs play nice with water. About 70% of new medicines being developed today are poorly soluble in water, which means they struggle to dissolve in your gut and enter your bloodstream. These are often labeled as BCS Class II or IV drugs-terms you don’t need to remember, but the outcome matters: without help, they pass through your body mostly unused. That’s where fat comes in. When you eat fatty foods, your body releases bile and digestive enzymes that break down fats into tiny droplets. These droplets act like molecular taxis, picking up poorly soluble drugs and carrying them into your system. The result? Absorption can jump by 20% to over 300%, depending on the drug. For example, the immunosuppressant cyclosporine (Neoral®) sees a 20-30% boost in absorption when taken with food compared to its older version, Sandimmune®.The Science Behind the Food Effect
The phenomenon is called the “food effect”-a well-documented interaction between what you eat and how your body handles medicine. Lipid-based formulations were developed to intentionally trigger this natural process. These aren’t just pills with added oil; they’re engineered systems designed to mimic the body’s own fat-digesting machinery. Most of these formulations use medium-chain triglycerides (MCTs), like those found in coconut oil. Why? Because MCTs break down faster than long-chain fats-within 15 to 30 minutes in the small intestine-compared to 60 to 90 minutes for fats from meat or butter. This speed matters. Faster breakdown means quicker formation of micelles (tiny fat bubbles) that trap the drug and keep it dissolved long enough to be absorbed. These systems also include surfactants (like Tween 80) and cosolvents (like Transcutol HP) that stabilize the mixture. Together, they create droplets between 100 and 300 nanometers wide-small enough to slip through the gut lining and into the bloodstream. The whole setup works best at the slightly alkaline pH of the small intestine (around 6.5-7.0), where bile salts are most active.Real-World Examples: When Fat Makes a Difference
Some medications simply don’t work without fat. Take itraconazole (Sporanox®), an antifungal used for stubborn infections. The capsule version absorbs poorly and varies wildly based on stomach acidity and food intake. But the liquid, lipid-based solution? It delivers 2.8 times more drug into the blood-even on an empty stomach-and cuts absorption variability by 40%. That’s the difference between a treatment that works and one that doesn’t. Fenofibrate (Tricor®), used to lower triglycerides, shows similar results. Patients on the lipid-based version report fewer stomach issues and need to take it only once a day instead of three. A 2022 study found 87% of users preferred it over the older version, and 72% said they noticed fewer side effects. Even cyclosporine, once notorious for needing strict timing with meals, became easier to manage when reformulated with lipids. Many transplant patients on Reddit have shared that switching to Neoral® eliminated the stress of planning meals around doses. One user wrote: “I don’t have to worry about whether my breakfast has enough fat anymore.”
When Fat Doesn’t Help-Or Makes Things Worse
This isn’t a universal rule. For drugs that dissolve easily in water (BCS Class I), like atenolol or metformin, fat has little to no effect. In fact, taking them with a heavy meal might slow absorption too much, delaying the drug’s onset. Some drugs actually need an acidic environment to dissolve. Bisphosphonates, used for osteoporosis, are a classic example. They require an empty stomach and no food for 30 minutes after taking them. Fat can interfere with their solubility in the stomach, reducing absorption and increasing the risk of esophageal irritation. And then there’s the issue of consistency. Not everyone digests fat the same way. People with cystic fibrosis, Crohn’s disease, or gallbladder removal may not produce enough bile. For them, even the best lipid-based drug might not work as intended. That’s why doctors often monitor blood levels closely for patients on these drugs.Cost, Convenience, and Trade-Offs
Lipid-based medications come with a price tag. Sporanox oral solution costs around $1,200 for a 30-day supply. The generic capsule version? About $300. That’s a 300% difference. Many patients, especially those without good insurance, end up choosing the cheaper option-even if it means dealing with unpredictable absorption or more side effects. Manufacturing these formulations is also more complex. They often require soft gelatin capsules to protect the lipid mix from air and moisture. This increases production costs by 25-35%. Only large pharmaceutical companies with specialized labs can reliably produce them. Smaller manufacturers often lack the technical know-how or equipment. Still, the trend is clear. In 2015, only 15% of new oral drugs for poorly soluble compounds used lipid-based systems. By 2023, that number jumped to 35%. Oncology, immunology, and antiviral drugs are leading the charge because many of these new compounds are inherently oily and hard to deliver.
What’s Next? Smarter, Personalized Lipid Pills
The future isn’t just about adding more fat-it’s about making fat work smarter. Researchers at MIT recently tested a “smart lipid capsule” that adjusts drug release based on real-time changes in gut pH and enzyme levels. Imagine a pill that knows when your body is ready to absorb it, and releases the drug only then. Another breakthrough came in March 2023 with Matinas BioPharma’s LNC platform, which delivered 92% bioavailability for the antifungal amphotericin B-nearly triple what traditional versions achieved. The FDA approved Vybar®, a new lipid-based fenofibric acid formulation, in 2022, showing 45% higher absorption with no food effect at all. These aren’t just lab curiosities. They’re real solutions for people who need reliable, consistent dosing. As plant-based lipids replace fish oil derivatives to meet sustainability goals, expect these systems to become even more accessible.What You Should Do
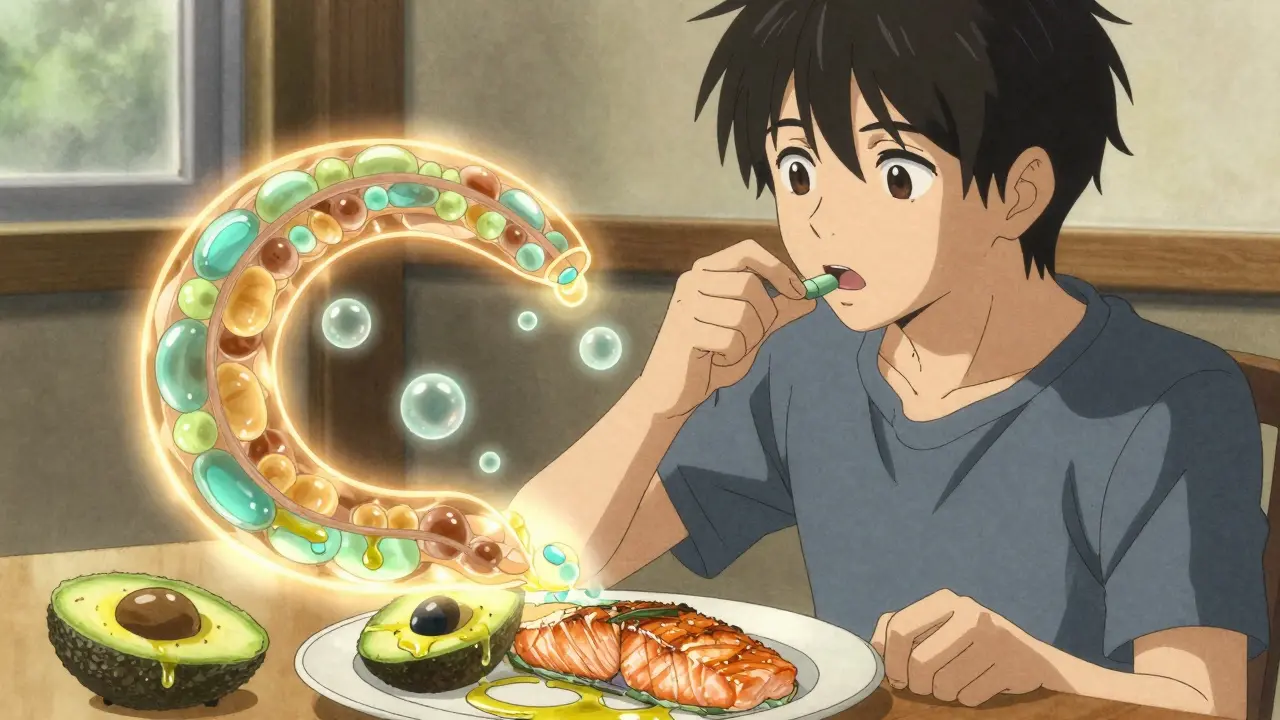
If you’re on a medication that’s known to interact with food, always check the label or ask your pharmacist. Some drugs say “take with food” for a reason. Others say “take on an empty stomach”-ignore that at your risk. Don’t assume all fats are equal. A handful of almonds won’t do the same job as a spoonful of MCT oil. But if your doctor recommends taking your pill with a meal, include some healthy fat: avocado, olive oil, nuts, or fatty fish. You don’t need a bacon cheeseburger-just enough fat to trigger the process. If you’re switching from a generic to a brand-name lipid-based version and notice fewer side effects or more consistent results, it’s not placebo. It’s science working the way it should.Final Thought
Fat isn’t the enemy of medicine-it’s sometimes its best ally. For millions of people taking drugs that barely dissolve in water, dietary fat turns a weak treatment into a powerful one. The next time you’re told to take your pill with food, don’t think of it as a restriction. Think of it as a partnership between your body and the science designed to help it.Do all medications need fatty foods to work?
No. Only medications that are poorly soluble in water-typically BCS Class II or IV drugs-benefit from fat. Common examples include cyclosporine, fenofibrate, itraconazole, and some HIV antivirals. Drugs like metformin or atenolol dissolve easily and don’t need fat to be absorbed.
Can I use any type of fat with lipid-based medications?
Not all fats are equally effective. Medium-chain triglycerides (MCTs), like those in coconut oil or specialized pharmaceutical oils, work best because they digest quickly and form effective micelles. While butter, avocado, or olive oil can help trigger the food effect, they’re less predictable than the engineered lipid systems in the medication itself. For maximum consistency, follow your doctor’s advice on meal composition.
Why do some lipid-based drugs cost so much more?
Lipid-based formulations require complex manufacturing, specialized ingredients, and protective packaging like soft gel capsules. They also undergo more rigorous testing to ensure stability and consistent absorption. These factors increase production costs by 25-35% compared to standard tablets or capsules, which is reflected in the price.
What happens if I take a lipid-based drug without fat?
You might not get enough of the drug into your bloodstream. For some medications, this can mean the treatment fails-like a transplant patient rejecting the organ, or a fungal infection coming back. In others, it just means you need a higher dose to achieve the same effect. Either way, it reduces reliability and increases risk.
Are there side effects from taking fat with medication?
Generally, no-unless you’re consuming excessive fat. Some people report mild bloating or diarrhea if they’re not used to high-fat meals. But the lipid-based formulation itself is designed to reduce side effects by allowing lower doses and smoother absorption. Many patients actually report fewer stomach issues with lipid versions compared to older, non-lipid ones.
Can I take lipid-based drugs with a keto or high-fat diet?
Yes, and it may even improve consistency. A steady intake of dietary fat helps maintain a predictable environment for absorption. However, if your diet changes drastically-say, switching from low-fat to high-fat-you should inform your doctor. Your blood levels might need monitoring, especially for drugs with narrow therapeutic windows like cyclosporine.
Do children or elderly patients respond differently to lipid-based drugs?
Children and older adults may have reduced bile production or slower digestion, which can affect how well lipid-based drugs work. Elderly patients with gallbladder issues or those on long-term antibiotics may also have altered gut flora that impacts fat digestion. Dosing may need adjustment, and caregivers should watch for signs the medication isn’t working-like recurring symptoms or lab value changes.
Is there a difference between prescription lipid formulations and over-the-counter fat supplements?
Yes. Prescription lipid formulations are precisely engineered with specific oils, surfactants, and ratios tested in clinical trials. Over-the-counter MCT oil or fish oil supplements aren’t designed for drug delivery. They might help a little, but they won’t reliably replicate the absorption boost you get from a properly formulated drug. Never substitute them without consulting your doctor.
