How to Measure Children’s Medication Doses Correctly at Home
 Dec, 11 2025
Dec, 11 2025
Getting the right dose of medicine for your child isn’t just important-it can be life-saving. A mistake of just one milliliter can mean the difference between healing and harm. Too little, and the infection won’t clear. Too much, and you could be rushing to the ER. The good news? Most errors aren’t caused by carelessness. They’re caused by confusion-over tools, units, and measurements that seem simple but aren’t.
Why Milliliters (mL) Are the Only Unit That Matters
Stop using teaspoons and tablespoons. Not because they’re "bad," but because they’re unreliable. A kitchen teaspoon can hold anywhere from 3.9 to 7.3 milliliters. That’s a 50% variation. For a child, that’s not a small error-it’s dangerous.
The CDC’s PROTECT initiative and the American Academy of Pediatrics both say the same thing: all pediatric liquid medications must be measured in milliliters (mL). No more "1 tsp," no more "½ tbsp." If the label says it, ignore it. Only trust numbers followed by "mL."
Here’s why this matters: 0.5 mL is not the same as 5 mL. That’s a tenfold difference. One parent gave their 18-month-old 5 mL of amoxicillin thinking it was 0.5 mL. The child ended up in intensive care. That kind of mistake happens more often than you think-about 7 in 10 parents mismeasure liquid meds at least once.
The Right Tools for the Job
Not all measuring tools are created equal. Here’s what works-and what doesn’t:
- Oral syringes (1-10 mL): The gold standard. Especially for doses under 5 mL. Accuracy rate: 94%. They let you see every drop, control the flow, and avoid spills.
- Dosing cups: Fine for older kids who can drink from a cup, but error rates jump to 68.5% for doses under 5 mL. Avoid if you’re giving less than a teaspoon.
- Droppers: Good for babies under 6 months. Usually 1-2 mL capacity. Make sure the tip fits snugly in the mouth to avoid leaks.
- Medication spoons: Only use if they’re labeled "5 mL" and come with the medicine. Household spoons? Never.
Studies show parents using oral syringes reduce dosing errors by 42% compared to those using cups or spoons. And if your child’s medicine comes with a syringe? Keep it. Don’t toss it. Don’t swap it for a cup "because it’s easier." It’s not.
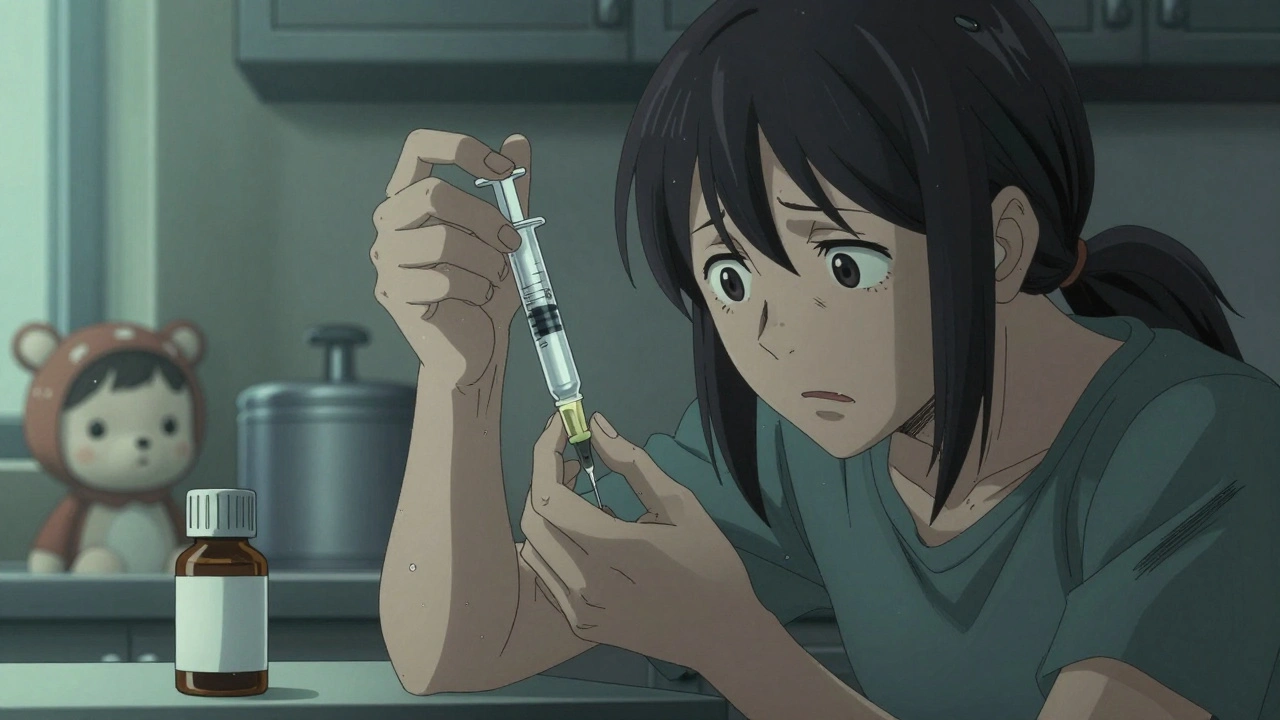
How to Measure Accurately (Step by Step)
Even the best tool won’t help if you don’t use it right. Here’s how to get it perfect every time:
- Read the label twice. Confirm the dose in mL-not teaspoons. Write it down if you need to.
- Use only the tool that came with the medicine. If it’s a syringe, use the syringe. Don’t grab a different one from the drawer.
- Hold the syringe vertically. Place it on a flat surface, eye-level. Look straight at the line. Don’t tilt it.
- Read the meniscus. The liquid forms a curve. Always read from the bottom of that curve.
- Draw slightly more than needed. Then gently push the plunger back to the exact line. This removes air bubbles.
- Give the dose slowly. Place the tip inside the cheek, not the front of the mouth. This reduces spitting.
Pro tip: If you give the same dose every day, mark the syringe with a permanent marker. A tiny dot at 2.5 mL? Saves time and stress.

Weight-Based Dosing: When the Prescription Says mg/kg
Many pediatric meds are dosed by weight: milligrams per kilogram (mg/kg). If your child weighs 22 pounds, that’s not 22 mg. It’s 10 kilograms (22 ÷ 2.2 = 10). Then you multiply: 40 mg/kg × 10 kg = 400 mg total per day.
Let’s say the doctor prescribes amoxicillin at 40 mg/kg/day in two doses. Your child is 22 lbs (10 kg). That’s 400 mg total. Split into two doses: 200 mg each. The bottle says 400 mg per 5 mL. So each dose is 2.5 mL.
Don’t guess. Use a calculator. Write it down. Double-check with the pharmacist. If the label says "100 mg/5 mL," and you need 200 mg, that’s 10 mL. Not 2 mL. Not 5 mL. 10 mL. Mistakes here are common-and deadly.
Common Mistakes Parents Make (And How to Avoid Them)
- Using kitchen spoons: 63% of parents admit to doing this before learning better. Stop. Now.
- Not shaking suspensions: Antibiotics like amoxicillin settle at the bottom. If you don’t shake the bottle for 10 seconds before each dose, your child gets only half the medicine. That’s how infections come back.
- Confusing mg and mL: One parent gave 10 mL of a 100 mg/5 mL solution thinking it was 10 mg. It was 200 mg. The child had a seizure. This happens more than you think.
- Using multiple caregivers without a system: Grandpa uses a spoon. Mom uses a syringe. Dad guesses. Chaos. Designate one person to give meds-or make a simple chart.
- Not checking expiration: Liquid antibiotics expire fast. Once opened, most last 14 days. After that, they lose potency.
What to Do When Your Child Refuses Medicine
68% of parents say their child spits out, coughs, or refuses medicine. Here’s what works:
- Use a syringe to squirt slowly into the cheek. Not the tongue. The back of the mouth.
- Mix with a small amount of apple sauce, yogurt, or juice. Only if the medicine allows it. Check the label or ask the pharmacist.
- Use flavored versions. Many pharmacies offer flavoring for prescriptions. Ask for strawberry, grape, or bubblegum.
- Don’t force it. If your child gags or chokes, stop. Wait 10 minutes. Try again. Stress makes it worse.

When to Call the Pharmacist or Doctor
You don’t have to figure it out alone. Call if:
- The label says "tsp" or "tbsp"-ask them to rewrite it in mL.
- The dose looks too high or too low for your child’s weight.
- The medicine looks different from last time.
- You’re unsure how to measure it.
Pharmacists are trained for this. They’ve seen it all. No question is too small. And if you’re not sure, you’re not alone.
Tools That Actually Help
There are smart tools now that make dosing foolproof:
- NurtureShot Color-Coded Syringes: Each color matches a common dose (e.g., blue = 2.5 mL). Reduces errors by 61%.
- Medisana BabyDos: A syringe with a built-in stopper to prevent over-dosing. Costs around £10.
- MedSafety App: Uses your phone’s camera to scan the bottle and shows you exactly how much to give. Works offline.
Hospitals in the U.S. and UK are starting to give these out at discharge. Ask your pharmacist if they have any to lend or sell.
Final Rule: When in Doubt, Don’t Guess
Every year, thousands of children are hospitalized because of dosing errors. Most of them are preventable. You don’t need to be a nurse. You just need to be careful.
Use the syringe. Read in mL. Shake the bottle. Double-check the math. Ask questions. Write it down. Keep the tool that came with the medicine.
Your child’s safety isn’t about being perfect. It’s about being consistent. One mistake can change everything. But one habit-using the right tool the right way-can save a life.
Can I use a kitchen teaspoon if I don’t have a syringe?
No. A kitchen teaspoon is not standardized. It can hold between 3.9 and 7.3 milliliters, while a proper 5 mL dose is exactly that. Using it risks under-dosing or overdosing your child. Always use the measuring tool that came with the medicine-preferably an oral syringe.
What if the prescription says "1 teaspoon" instead of mL?
Call the pharmacy or doctor immediately and ask them to rewrite the prescription in milliliters (mL). The CDC and American Academy of Pediatrics have banned the use of teaspoons for children’s meds because they cause dangerous errors. You have the right to ask for a clear, metric-only label.
How do I know if I’m giving the right dose based on my child’s weight?
Convert pounds to kilograms by dividing by 2.2. Then multiply the weight in kg by the dose prescribed per kg. For example, if your child weighs 22 lbs (10 kg) and the dose is 15 mg/kg, you give 150 mg total. If the medicine is 100 mg per 5 mL, that’s 7.5 mL. Always double-check with your pharmacist before giving the first dose.
Why does my child’s liquid medicine need to be shaken before each use?
Many liquid medications, especially antibiotics, are suspensions. The active ingredient settles at the bottom. If you don’t shake the bottle for 10-15 seconds before each dose, your child gets less medicine-sometimes only half. That can cause the infection to return or become resistant. Always shake well before measuring.
Are there apps that can help me measure doses correctly?
Yes. Apps like MedSafety use your phone’s camera to scan the medicine bottle and show you the exact dose in mL. Some even guide you through the measuring process with augmented reality. These tools have been shown to reduce dosing errors by over 50% in clinical trials. Download one and use it until you feel confident.
What should I do if I think I gave the wrong dose?
Call your pediatrician or poison control immediately. Do not wait for symptoms. Even if your child seems fine, some overdoses take hours to show signs. Have the medicine bottle handy when you call. Tell them the name of the medicine, the dose you gave, your child’s weight, and the time it was given. It’s better to be safe than sorry.

Donna Anderson
December 12, 2025 AT 19:54OMG I just realized I’ve been using a kitchen spoon for my kid’s amoxicillin 😳 Thanks for this post-I’m buying syringes today.