Inflammation and Gut Health: Understanding the Critical Connection
 Oct, 18 2025
Oct, 18 2025
Inflammation Diet Score Calculator
This tool calculates your diet's impact on inflammation based on the article's research. Select foods you consume regularly to get a personalized score and recommendations.
Select Your Foods
Anti-Inflammatory Foods
Pro-Inflammatory Foods
Quick Takeaways
- Chronic inflammation can damage the gut lining and alter the microbiome.
- Leaky gut often results from an overactive immune response in the intestine.
- Foods rich in fiber, omega‑3s, and fermented products help calm inflammation.
- Regular movement, stress management, and adequate sleep are non‑dietary levers.
- Persistent gut symptoms merit a professional evaluation for underlying inflammatory disorders.
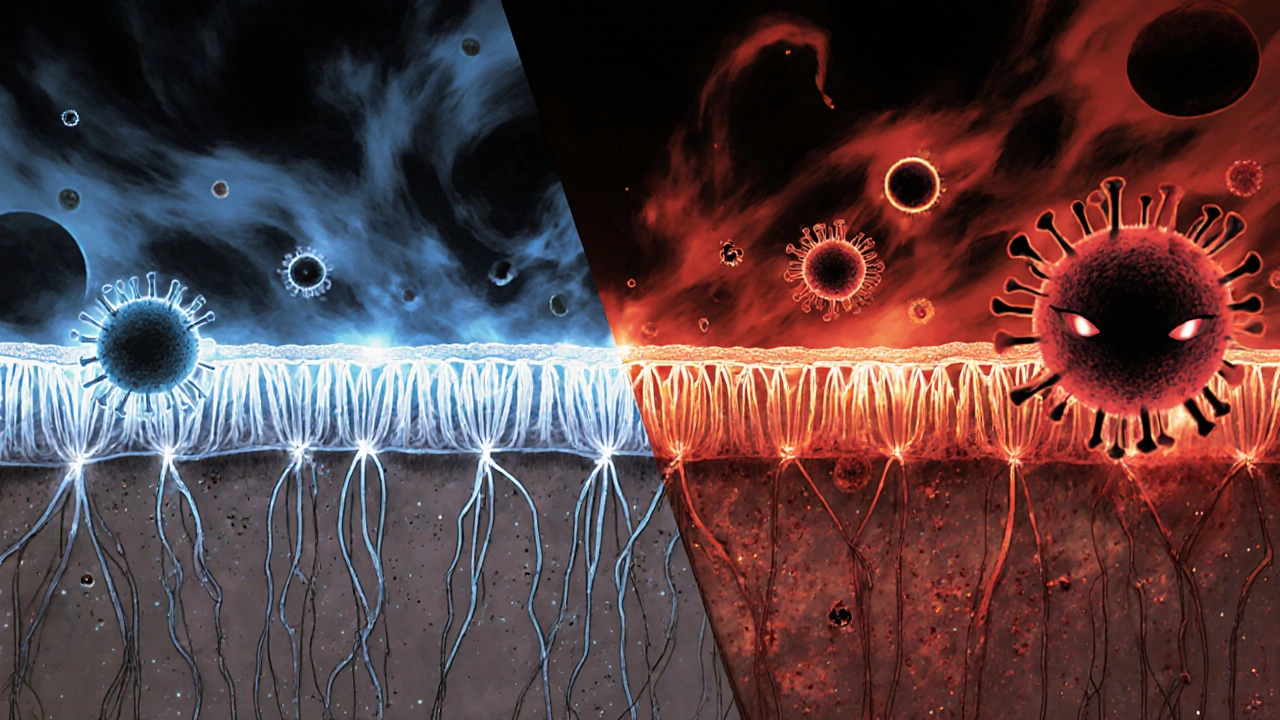
When inflammation and gut health collide, the result is a cascade that can influence everything from mood to metabolism. This guide walks you through what inflammation really means, how it messes with your gut, and practical steps you can take today to restore balance.
What is Inflammation?
Inflammation is the body’s natural alarm system, a rapid response designed to isolate and eliminate harmful agents such as pathogens, damaged cells, or irritants. Once a threat is detected, immune cells flood the area, releasing signaling proteins called cytokines. In the short term, this response is protective, promoting healing and clearing debris.
Problems arise when the alarm stays on. Chronic inflammation keeps the gut’s immune environment on high alert, eroding the protective mucus layer, disrupting tight junctions, and skewing the composition of the gut microbiome. Over time, this can lead to leaky gut, nutrient malabsorption, and heightened risk for conditions like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and even metabolic syndrome.
The Gut Microbiome: Your Internal Ecosystem
The gut microbiome is a dense community of bacteria, fungi, viruses, and archaea that call your intestines home. In a healthy state, these microbes perform essential jobs: they ferment indigestible fibers into short‑chain fatty acids (SCFAs) like butyrate, synthesize certain vitamins, and train the immune system to tolerate harmless substances.
When inflammation disturbs this balance-a condition known as dysbiosis-beneficial species shrink while opportunistic, pro‑inflammatory microbes flourish. The result is a feedback loop: dysbiosis fuels more cytokine production, which in turn worsens gut permeability.
How Inflammation Damages the Gut Lining
The intestinal wall is lined with epithelial cells tightly sealed by protein complexes called tight junctions. These junctions act like a security gate, allowing nutrients through while keeping toxins out. Pro‑inflammatory cytokines such as tumor necrosis factor‑alpha (TNF‑α) and interleukin‑6 (IL‑6) can loosen these junctions, creating a condition popularly called “leaky gut.”
Leaky gut lets partially digested food particles, bacterial fragments, and endotoxins slip into the bloodstream. The immune system interprets this as a threat, launching another wave of inflammation-often manifesting as joint pain, skin rashes, or brain fog. This systemic spillover explains why gut issues frequently mirror symptoms in distant organs.

Key Triggers of Gut‑Driven Inflammation
- Dietary culprits: excess refined sugars, trans fats, and processed meat can promote the growth of pro‑inflammatory bacteria.
- Frequent use of non‑steroidal anti‑inflammatory drugs (NSAIDs) can irritate the intestinal lining directly.
- Chronic stress elevates cortisol, which in turn impairs the gut barrier and alters microbial diversity.
- Insufficient sleep disrupts the circadian rhythm of gut microbes, reducing SCFA production.
- Environmental toxins, such as pesticides, can damage the microbiome and trigger immune activation.
Anti‑Inflammatory Diet: Food as Medicine
What you eat is the most direct lever you have over both inflammation and microbiome health. Below is a simple comparison of pro‑ and anti‑inflammatory food groups.
| Category | Pro‑Inflammatory | Anti‑Inflammatory |
|---|---|---|
| Fats | Trans fats, refined vegetable oils | Olive oil, avocado oil, omega‑3 rich fish |
| Carbohydrates | White bread, sugary drinks | Whole grains, legumes, low‑glycemic fruits |
| Proteins | Processed meats, excess red meat | Fatty fish (salmon, mackerel), poultry, plant‑based proteins |
| Fermented | None | Yogurt, kefir, sauerkraut, kimchi |
| Fiber Sources | Low‑fiber refined foods | Vegetables, nuts, seeds, chia, flax |
Key nutrients that actively suppress inflammatory pathways include:
- Omega‑3 fatty acids (EPA, DHA) found in oily fish and algae supplements.
- Polyphenols from berries, green tea, and dark chocolate, which modulate gut bacteria.
- Short‑chain fatty acids produced when fiber‑rich foods are fermented by beneficial microbes.
Practical Steps to Calm Gut Inflammation
- Increase daily fiber intake to 25‑30 g by adding beans, lentils, broccoli, and berries.
- Include at least two servings of fatty fish per week or consider a high‑quality algae‑based omega‑3 supplement.
- Introduce fermented foods (a handful of yogurt, kefir, or kimchi) to boost probiotic populations.
- Swap refined carbs for whole‑grain alternatives like quinoa, steel‑cut oats, or brown rice.
- Limit NSAID use; when pain relief is needed, opt for acetaminophen or discuss alternatives with a clinician.
- Practice stress‑reduction techniques-mindful breathing, short walks, or a 10‑minute meditation.
- Prioritize 7‑9 hours of sleep; maintain a consistent bedtime schedule.
- Stay hydrated; aim for at least 2 L of water daily to support mucosal health.
These actions target the root causes-excess cytokine production, compromised tight junctions, and microbial imbalance-rather than just masking symptoms.

When to Seek Professional Help
If you notice any of the following, it’s time to book an appointment with a gastroenterologist or a functional medicine practitioner:
- Persistent abdominal pain or cramping lasting more than three weeks.
- Unexplained weight loss, chronic fatigue, or night sweats.
- Frequent diarrhea or constipation that disrupts daily life.
- Blood in stool, severe bloating, or sudden changes in bowel habits.
Doctors may order blood tests for C‑reactive protein (CRP) and fecal calprotectin to gauge inflammation levels, as well as stool analyses to map your microbiome composition. In some cases, targeted probiotic prescriptions or low‑FODMAP diets are recommended.
Future Directions: Healing the Gut at the Molecular Level
Research in 2024-2025 is zeroing in on post‑biotics-bioactive compounds produced by beneficial microbes-as a next‑generation therapy. Early trials show that butyrate supplements can restore tight‑junction integrity in animal models of leaky gut. Meanwhile, personalized nutrition platforms use AI to match dietary recommendations with an individual’s unique microbiome fingerprint, promising more precise anti‑inflammatory strategies.
While these innovations are still emerging, the fundamentals remain unchanged: reduce chronic triggers, nourish the microbiome, and support the body’s natural repair mechanisms.
Frequently Asked Questions
Can I reverse leaky gut on my own?
Yes, many people see improvement by cutting inflammatory foods, adding fiber‑rich meals, and incorporating fermented probiotic sources. Consistency over weeks is key.
Are all probiotics the same?
No. Strains differ in their ability to survive stomach acid and in the specific benefits they offer. Lactobacillus rhamnosus GG, for example, is well‑studied for gut barrier support, while Bifidobacterium longum excels at reducing inflammation.
Do NSAIDs always hurt the gut?
Regular, high‑dose use can damage the intestinal lining, especially in people with pre‑existing gut issues. Intermittent, low‑dose use is less risky, but alternatives should be explored.
What is the best source of omega‑3 for gut health?
Fatty fish like salmon, sardines, and mackerel provide EPA and DHA, the forms most effective at reducing cytokine production. For vegetarians, algae‑based supplements are a comparable alternative.
How quickly can diet changes affect inflammation?
Markers such as CRP can drop within 2‑4 weeks of adopting an anti‑inflammatory diet, while microbiome balance may take 6‑12 weeks for noticeable improvements in symptoms.

Alex Lineses
October 18, 2025 AT 12:39First, kudos for diving deep into the immunological cascade that underpins gut inflammation. When you consider the cytokine milieu-particularly TNF‑α, IL‑6, and IL‑1β-you’re really looking at a complex network of signal transduction pathways that modulate epithelial tight‑junction integrity. Chronic activation of NF‑κB, for instance, perpetuates a feed‑forward loop that degrades mucosal barrier proteins such as claudin‑1 and occludin. This is why patients with sustained dysbiosis often present with heightened systemic endotoxemia, a phenomenon colloquially termed “leaky gut.”
From a therapeutic standpoint, the first order of business is to attenuate that cytokine surge. Dietary omega‑3 fatty acids competitively inhibit the arachidonic acid cascade, thereby reducing prostaglandin E2 synthesis. Concurrently, fermentable fibers act as prebiotic substrates, fostering the growth of SCFA‑producing taxa like Faecalibacterium prausnitzii. SCFAs such as butyrate serve as histone deacetylase inhibitors, which promote regulatory T‑cell differentiation and reinforce epithelial restitution.
In practice, I advise patients to incorporate at least 25 g of soluble fiber per day-think oatmeal, chia seeds, and legumes-paired with two servings of oily fish or a high‑quality algae supplement. Adding a daily probiotic containing Lactobacillus rhamnosus GG can further stabilize the mucosal immune environment by outcompeting opportunistic Gram‑negative organisms.
Equally important are non‑nutritional levers: circadian‑aligned sleep, moderate aerobic activity, and mindfulness‑based stress reduction have demonstrable effects on cortisol‑mediated gut permeability. In my experience, a 30‑minute brisk walk after dinner can shift the gut microbial diurnal rhythm toward increased SCFA output.
Finally, monitor biomarkers such as CRP and fecal calprotectin every 4–6 weeks to gauge response. A downward trend often precedes symptomatic improvement, underscoring the value of objective data in guiding iterative diet and lifestyle tweaks. Stay consistent, personalize the plan to your microbiome profile, and remember that the gut‑immune axis thrives on balance, not deprivation.
Brian Van Horne
October 20, 2025 AT 06:19In summation, a measured, evidence‑based regimen remains the cornerstone of gut health.
Norman Adams
October 21, 2025 AT 23:59Oh, delightfully, you’ve managed to regurgitate the same textbook blather about cytokines and tight junctions that even a second‑year immunology undergrad could recite, as if we’re all perched on the edge of some groundbreaking revelation. One might wonder why the author felt compelled to embellish the narrative with buzzwords like “feed‑forward loop” and “SCFA‑mediated epigenetic modulation” when the underlying premise is simply “eat your veggies and stop taking ibuprofen.” The irony is palpable: a piece ostensibly aimed at the layperson is drenched in jargon that would make a graduate‑level seminar blush.
Margaret pope
October 23, 2025 AT 17:39You are spot on the gut microbiome is key and adding fiber and omega‑3s does help keep inflammation down they really support the barrier function and overall health
Joe Moore
October 25, 2025 AT 11:19Yo you think this is just science but what they dont tell u is that big pharma is pushin these “omega‑3 supplements” as a way to keep us dependent on their pricey products while the real cure is hidden in ancient fermented foods that got banned by the elites dont be fooled the whole system is rigged and the gut is just the entry point for them to control our minds
Ayla Stewart
October 27, 2025 AT 03:59I appreciate the encouragement and would add that tracking fiber intake with a simple food diary can make the process more concrete for many people.
James Mali
October 28, 2025 AT 21:39Well, after reading all that, I guess the gut is just another metaphor for how we try to fill the void inside, but honestly, if you’re not willing to give up the processed snacks, no amount of fancy science is going to fix it.
Janet Morales
October 30, 2025 AT 15:19Enough with the fatalistic drivel! You’re choosing despair over agency and letting an excuse for laziness masquerade as “philosophy.” Take charge, overhaul your diet, and stop wallowing in self‑pity.