Lithium and NSAIDs: Understanding the Dangerous Nephrotoxicity Risk
 Dec, 29 2025
Dec, 29 2025
Lithium-NSAID Toxicity Calculator
Lithium-NSAID Interaction Risk Calculator
This tool estimates how NSAIDs may affect your lithium levels and potential toxicity risk. Remember: Always consult your doctor before making medication changes.
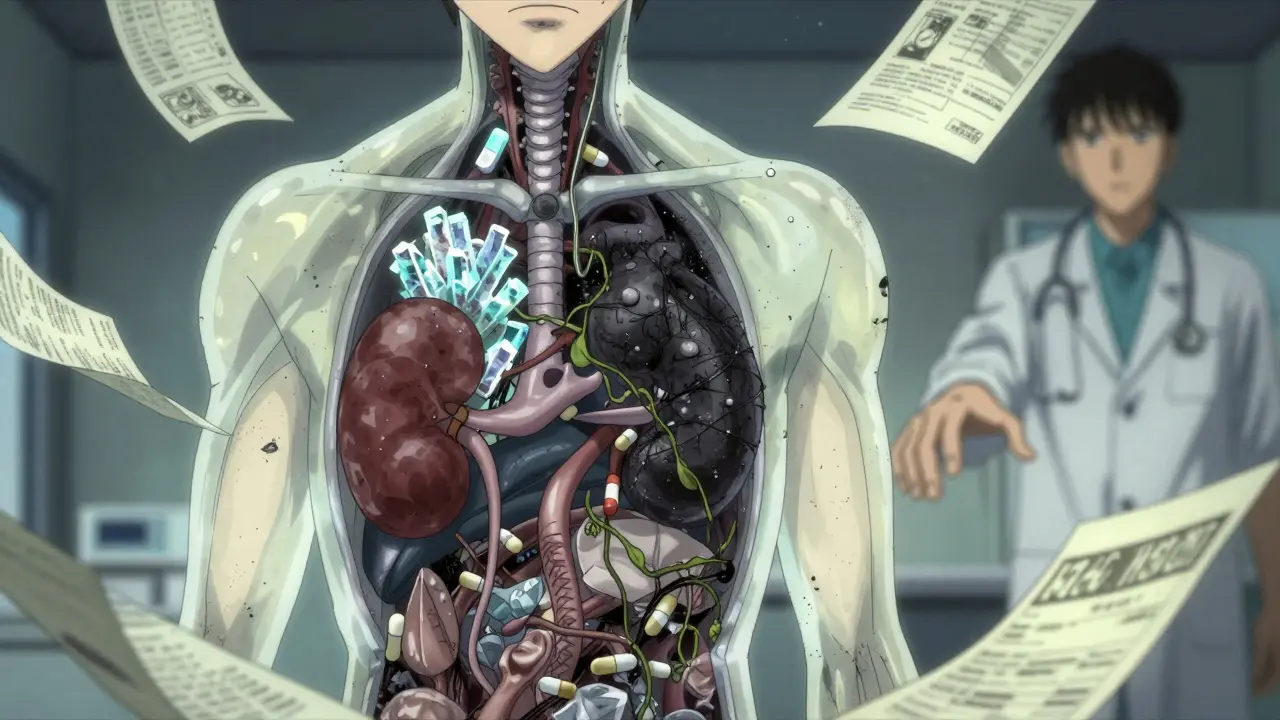
Many people with bipolar disorder rely on lithium to keep their moods stable. It’s been used for over 50 years and remains one of the most effective treatments we have. But if you’re taking lithium and reach for an over-the-counter painkiller like ibuprofen or naproxen, you could be putting your kidneys - and your life - at serious risk. This isn’t a rare side effect. It’s a well-documented, predictable, and often overlooked interaction that can lead to hospitalization, permanent kidney damage, or even death.
How Lithium and NSAIDs Interact
Lithium is cleared from your body almost entirely by your kidneys. It’s filtered out through the glomeruli and then partially reabsorbed in the renal tubules. That’s where NSAIDs come in. These drugs - including common ones like ibuprofen, naproxen, and indomethacin - block enzymes called COX-1 and COX-2. Those enzymes help produce prostaglandins, which keep blood flowing to your kidneys. When NSAIDs shut down prostaglandin production, your kidneys get less blood. That means they can’t filter lithium as well.
The result? Lithium builds up in your blood. Studies show NSAIDs can reduce lithium clearance by 25% to 60%. That’s not a small change. A normal lithium level is between 0.6 and 1.0 mmol/L. Go above 1.5 mmol/L, and you’re in toxic territory. Levels above 2.0 mmol/L can cause seizures, coma, or death. And this doesn’t take weeks to happen. Toxicity can develop within 48 to 72 hours after starting an NSAID.
Why This Interaction Is So Dangerous
It’s not just about lithium levels rising. The combination also damages your kidneys directly. Lithium itself can cause long-term kidney changes - it interferes with how kidney cells handle water and salt. NSAIDs make this worse by reducing blood flow and causing ischemic injury. Together, they create a one-two punch. A 2023 study in JAMA Network Open found that people taking both drugs had a 3.2 times higher risk of acute kidney injury than those on lithium alone. The risk was even higher - nearly five times - in the first 30 days after starting the NSAID.
And it’s not just acute injury. Over time, this combo accelerates chronic kidney disease. One study tracking over 12,000 patients found that those on lithium and NSAIDs had a 2.8 times higher rate of eGFR decline - meaning their kidney function dropped faster - than those on lithium alone. People with existing kidney problems (eGFR below 60 mL/min) are at the highest risk. Their kidneys can’t compensate at all.
Not All NSAIDs Are Equal
Some NSAIDs are worse than others. Indomethacin can spike lithium levels by 40% to 60%. Piroxicam and naproxen raise them by 25% to 35%. Ibuprofen, the most commonly used, increases levels by 20% to 30%. Even celecoxib - often called a “kidney-friendly” NSAID - still raises lithium by 10% to 15%, especially if your kidneys are already impaired.
Aspirin and low-dose aspirin are different. They don’t significantly affect lithium levels. But that doesn’t mean they’re safe for everyone. High-dose aspirin can still cause problems. And don’t assume that because something is “over-the-counter,” it’s harmless. The biggest danger isn’t the drug itself - it’s that most people don’t realize it’s dangerous.
What About Acetaminophen or Opioids?
If you need pain relief while on lithium, acetaminophen (Tylenol) is your safest bet. It doesn’t interfere with kidney function or lithium clearance. Studies show it causes less than a 5% change in lithium levels. That’s negligible. The catch? Don’t exceed 3,000 mg per day. Higher doses can damage your liver, especially if you drink alcohol or have existing liver issues.
Opioids like tramadol or codeine are a second option. They don’t directly affect lithium levels, but they can cause dehydration - which indirectly raises lithium concentration. If you must use them, start low, go slow, and drink plenty of fluids. Avoid opioids that cause constipation or drowsiness if you’re already prone to those side effects from lithium.
But avoid NSAIDs entirely if you can. Even short-term use - like taking ibuprofen for a headache or sore knee - can trigger toxicity. And the damage doesn’t disappear when you stop the NSAID. Prostaglandin suppression lasts 7 to 10 days. Your lithium levels may stay elevated for over a week after you stop the painkiller.
Who’s Most at Risk?
Age is a major factor. Over half of lithium-NSAID related kidney injuries happen in people over 65. Why? Kidney function naturally declines with age. Many older adults also take diuretics, ACE inhibitors, or have diabetes - all of which further strain the kidneys. A 2023 study of 478 nephrology clinics found that 52% of lithium-related acute kidney injuries occurred in patients over 65.
Another big risk group: people seeing multiple doctors. If you see a primary care provider for back pain, a rheumatologist for arthritis, and a psychiatrist for bipolar disorder, chances are one of them doesn’t know you’re on lithium. A 2023 study found that only 58% of primary care doctors knew NSAIDs were high-risk for lithium users. That’s not a failure of the patient - it’s a failure of communication.
And then there’s the Reddit effect. In one thread with 127 patient reports, 70% said they took ibuprofen without being warned. Nearly a third were prescribed the NSAID by a doctor who didn’t know about their lithium use. That’s terrifying - and completely preventable.
What Should You Do?
If you’re on lithium:
- Never take NSAIDs without talking to your psychiatrist or nephrologist. Even one dose can be dangerous.
- Use acetaminophen instead. It’s safe, effective, and widely available.
- Hydrate. Drink at least 2 to 3 liters of water daily, especially if you’re sick, sweating, or traveling.
- Know the signs of toxicity. Tremors, nausea, vomiting, diarrhea, confusion, muscle weakness, slurred speech, or seizures - these aren’t normal side effects. They’re red flags.
- Get your lithium levels checked. If you must take an NSAID (and you shouldn’t), your doctor should check your levels within 48 to 72 hours and again after a week.
- Ask for a written warning. If your doctor prescribes an NSAID, demand they document the risk and your understanding of it. If they don’t, get a second opinion.

What Doctors Should Be Doing
Guidelines from the American Psychiatric Association, the American Society of Nephrology, and the European Psychiatric Association all agree: avoid NSAIDs in lithium users whenever possible. If absolutely necessary, monitor lithium levels twice a week and kidney function weekly for the first month.
But here’s the problem: most clinics don’t follow this. A 2021 audit found only 62% of lithium-prescribing clinicians included NSAID warnings in patient education materials. Compare that to 99% who warned about diuretics - drugs that also interact with lithium. Why the gap? Because NSAIDs are so common, people assume they’re harmless.
Some hospitals are fixing this. Kaiser Permanente reduced co-prescribing from 32% to 12% by adding hard alerts in their electronic system and requiring provider education. The Veterans Health Administration only saw a 15% drop - proof that alerts alone aren’t enough. You need training, policy, and culture change.
The FDA now requires a boxed warning on lithium labels about NSAID interactions. But warnings on a label don’t help if the prescriber doesn’t read them. What’s needed are electronic health record systems that block NSAID prescriptions for lithium users unless a nephrologist signs off.
The Bigger Picture
This isn’t just about one drug interaction. It’s about how our healthcare system treats mental health. People with bipolar disorder are often treated by specialists, but their physical health - pain, blood pressure, arthritis - is managed by others. The system doesn’t talk to itself. And patients pay the price.
Every year, lithium-NSAID interactions cost the U.S. healthcare system nearly $50 million in hospitalizations. Each episode averages over $18,000. And for many patients, the damage is permanent. One study found that 35% of those hospitalized for lithium toxicity after NSAID use developed permanent kidney damage.
There’s hope. A 2023 clinical trial tested a new drug that mimics prostaglandins to protect kidney blood flow without affecting lithium clearance. Early results showed an 87% reduction in lithium level spikes. That could be a game-changer.
But until then, the safest choice is simple: if you’re on lithium, skip the ibuprofen. Use acetaminophen. Drink water. Talk to your doctor. And if your doctor prescribes an NSAID, ask: “Do you know I’m on lithium?” If they hesitate - walk out and find someone who knows better.
What If You’ve Already Taken an NSAID?
If you took an NSAID for a day or two and didn’t know about the interaction:
- Stop the NSAID immediately.
- Drink extra water - at least 2 to 3 liters over the next 24 hours.
- Call your psychiatrist or pharmacist. Don’t wait for symptoms.
- Get a lithium blood test within 48 hours.
- Watch for tremors, confusion, or nausea. If they appear, go to the ER.
Most people recover fully if caught early. But delay can mean permanent damage.

Manan Pandya
December 30, 2025 AT 00:31Lithium and NSAIDs is one of those silent killers in psych care. I’ve seen patients end up in the ER over a weekend ibuprofen for a headache. No one warned them. No one thought it mattered. It’s not just about the numbers-it’s about how normal people assume OTC means safe. This needs to be shouted from the rooftops.
Nisha Marwaha
December 30, 2025 AT 10:31The pharmacokinetic interaction is unequivocally mediated by COX-2 inhibition-induced reduction in renal perfusion, leading to diminished glomerular filtration rate and subsequent decreased lithium excretion. The resultant hypernatremia and volume contraction exacerbate tubular reabsorption, culminating in toxic serum concentrations. Clinically, this represents a Class I drug-drug interaction with high morbidity potential, particularly in geriatric populations with age-related nephron loss and polypharmacy.
Paige Shipe
December 31, 2025 AT 15:43I’m sorry but this is why people shouldn’t be on lithium in the first place. It’s a dangerous drug with too many stupid rules. If you can’t take a painkiller without risking your life, maybe you’re not stable enough to be on it. Acetaminophen? Really? That’s the best we can do? I’ve seen people get liver failure from Tylenol too. This whole system is broken.
Nicole K.
January 1, 2026 AT 08:04You’re telling me I can’t take Advil for my cramps? That’s ridiculous. My doctor never said anything about this. I’ve been on lithium for 8 years and I’ve taken ibuprofen every month. Nothing happened. So why are you scaring people? You’re just trying to make money off fear. I’m not falling for it.
Amy Cannon
January 2, 2026 AT 10:40As someone who has lived with bipolar disorder for over two decades, I must say that the cultural context surrounding psychiatric medication safety is profoundly inadequate in the United States. The normalization of over-the-counter pharmaceuticals as benign substances, coupled with a fragmented healthcare infrastructure, creates a perfect storm for iatrogenic harm. It is not merely a pharmacological issue-it is a systemic failure of interprofessional communication, patient education, and institutional accountability. One must ask: who bears responsibility when the algorithm fails to flag a contraindication? The physician? The pharmacist? The patient? Or the entire edifice of capitalist medicine?
Himanshu Singh
January 4, 2026 AT 02:44Man this is so important. I just found out my buddy took naproxen for his back and ended up in the hospital. He didn’t even know. I told him to always ask his doc before taking anything. Seriously, if you’re on lithium, just stick with Tylenol. And drink water. I know it sounds simple but it saves lives. Thanks for posting this!
Jasmine Yule
January 5, 2026 AT 03:41This is why we need better mental health advocacy. People with bipolar disorder are often treated like they’re fragile, but the truth is they’re being failed by a system that doesn’t connect the dots. I’m so tired of seeing patients get hurt because no one talked to each other. I’ve been there-I’ve had to fight to get my own meds adjusted. If you’re on lithium, you deserve better than guesswork. And if you’re a doctor? Stop assuming patients know the risks. Educate them. Like, really educate them.
Lisa Dore
January 6, 2026 AT 00:54I’m so glad someone finally put this out there. My sister has been on lithium for 15 years. She never knew about the NSAID risk until she got sick last year. Now she carries a card in her wallet that says ‘LITHIUM USER-NO NSAIDS’. She even made a little sticker for her phone case. Small things matter. We need more of this. Not just warnings-action. Like, real action.
Sharleen Luciano
January 7, 2026 AT 05:56It’s amusing how the general public treats psychiatric medication like a magic pill without understanding its biological consequences. Lithium is not a vitamin. It’s a heavy metal with a narrow therapeutic index. The fact that people casually take NSAIDs without consulting a specialist speaks volumes about the erosion of medical literacy. If you’re not willing to learn the pharmacology of your own treatment, perhaps you shouldn’t be on it. This isn’t about fear-it’s about responsibility.
Alex Ronald
January 8, 2026 AT 10:27Just wanted to add that if you’re on lithium and need pain relief, don’t forget about topical NSAIDs like diclofenac gel. They’re absorbed minimally and usually don’t affect serum lithium levels. Also, cold packs, physical therapy, and even acupuncture can help with chronic pain without the risk. I’m a nurse and I see this happen way too often. Knowledge is power-share this.
Teresa Rodriguez leon
January 9, 2026 AT 06:31Why do people always act like they’re the first to find out about this? I’ve been on lithium since I was 19. I’ve had three kidney function tests because I took ibuprofen once. I’m not mad-I’m just tired of the same drama over and over. Just stop. Use Tylenol. Drink water. Be smart. That’s it.
Aliza Efraimov
January 10, 2026 AT 02:57I’m a nephrologist and I’ve seen this exact scenario 17 times in the last year alone. One patient, 72, took ibuprofen for arthritis. Lithium level went from 0.8 to 2.7 in 72 hours. He had seizures. Survived, but now needs dialysis. This isn’t theoretical. It’s happening every day. If your doctor prescribes an NSAID, say: ‘I’m on lithium. Is this safe?’ If they don’t know, ask for a consult. Your kidneys aren’t replaceable.
Tamar Dunlop
January 10, 2026 AT 09:24In Canada, we’ve implemented mandatory electronic alerts in all provincial e-prescribing systems for lithium patients. If a clinician attempts to prescribe an NSAID, a pop-up appears requiring them to acknowledge the risk, document patient understanding, and confirm consultation with a psychiatrist. Since 2021, co-prescribing has dropped by 68%. This is not rocket science-it’s systemic design. We must stop relying on patient memory and start designing systems that protect them.
David Chase
January 11, 2026 AT 12:12AMERICA IS WEAK. We let people die because they took Advil. Meanwhile, in REAL countries, they don’t even sell NSAIDs over the counter. You need a prescription. Why? Because we don’t trust people to be responsible. And guess what? It works. You want to live? Stop being lazy. Stop taking random pills. If you’re on lithium, you’re not a normal person. You’re a medical case. Act like it. 🇺🇸💔💊