Medication-Induced Thrombotic Thrombocytopenic Purpura: A Life-Threatening Reaction You Need to Know
 Jan, 17 2026
Jan, 17 2026
TTP Risk Calculator
Medication Risk Assessment
TTP is a life-threatening blood disorder that can be triggered by certain medications. This tool helps assess your risk based on medications you're taking.
TTP Risk Assessment Result
Key Symptoms to Watch For:
- Sudden, unexplained bruising or tiny red dots on skin (petechiae)
- Extreme fatigue that doesn't go away
- Dark or tea-colored urine
- Confusion, headaches, slurred speech, or seizures
- Shortness of breath or chest pain without heart disease history
Drug-induced thrombotic thrombocytopenic purpura isn’t just a rare side effect-it’s a medical emergency that can kill within days if missed. It doesn’t come with a warning label you can easily spot. One minute you’re taking a common pill for a leg cramp or a heart condition; the next, your platelets crash, your red blood cells shatter, and your brain or kidneys start failing. This isn’t a theoretical risk. It’s happened to people who drank tonic water every night, took daily aspirin alternatives, or followed standard transplant protocols. And too often, doctors mistake it for something else-flu, ITP, sepsis-until it’s too late.
What Exactly Is Drug-Induced TTP?
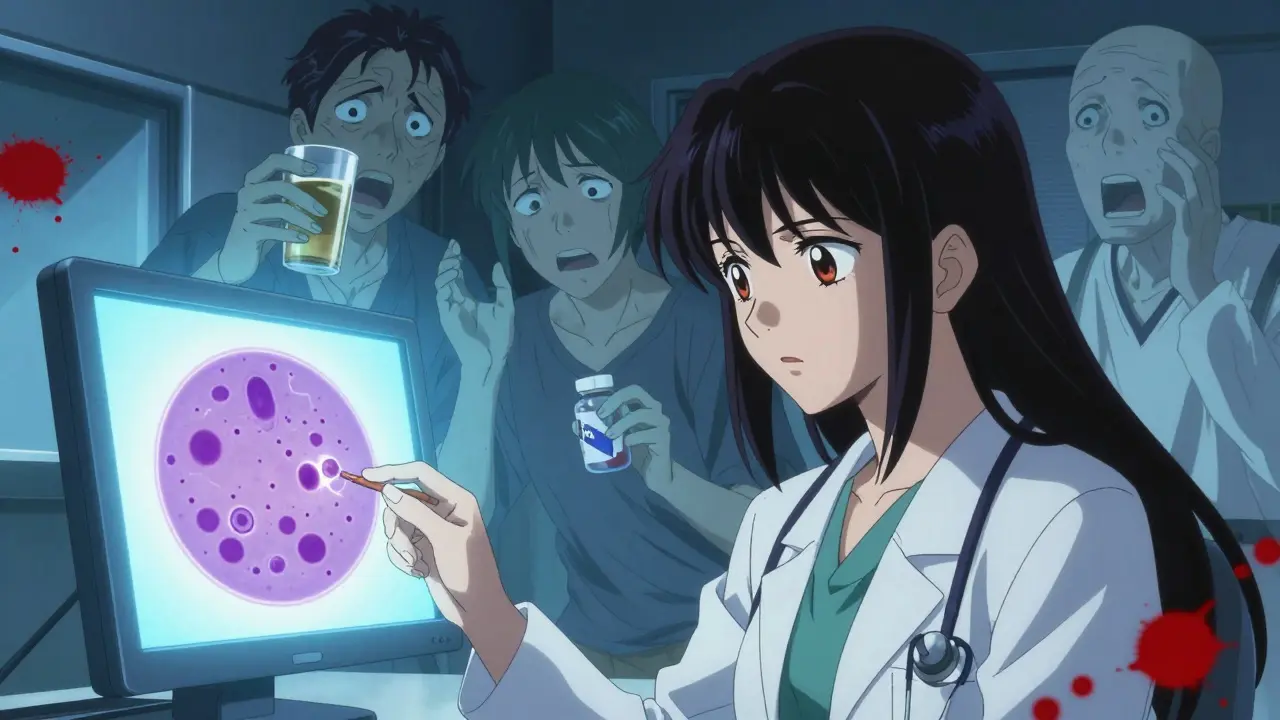
Thrombotic thrombocytopenic purpura (TTP) is a blood disorder where tiny clots form throughout small blood vessels. These clots chew up platelets, leaving you with dangerously low counts. They also tear apart red blood cells as they squeeze through the blocked vessels, causing anemia. The result? Bruising, fatigue, confusion, dark urine, kidney trouble, and sometimes seizures or stroke. The hallmark signs are low platelets (under 50,000/µL), schistocytes (fragmented red blood cells) on a blood smear, and high LDH levels with no haptoglobin.
What makes drug-induced TTP different from the inherited kind is the trigger: a medication. More than 300 drugs have been linked to it, but only about 20 have strong, proven ties. The two main ways drugs cause TTP are through immune reactions or direct toxicity.
Two Ways Medications Trigger TTP
Immune-mediated TTP (about 60% of cases) happens when your body makes antibodies that stick to your platelets-but only when the drug is around. Think of it like a lock and key. The drug is the key that turns the lock, letting the antibody bind and destroy your platelets. This is why you can take the drug once, recover, and be fine for years-until you take it again. Then, boom. Symptoms can show up in as little as 24 hours after re-exposure.
Dose-dependent TTP (about 40%) is slower and more predictable. It’s not an immune reaction. It’s physical damage. Drugs like cyclosporine and mitomycin C build up in your body over months, slowly injuring the lining of your blood vessels. Symptoms usually appear after 6 to 12 months of use. This type doesn’t respond as well to plasma exchange. Stopping the drug is the only real fix.
Top 5 Drugs Linked to TTP
Not all drugs carry the same risk. Based on decades of case reports and clinical data, these five have the strongest evidence:
- Quinine-found in tonic water and some leg cramp meds. One case per 10,000 prescriptions. Can strike within days. Even 2-3 glasses of tonic water daily for weeks has caused TTP.
- Clopidogrel (Plavix)-a common antiplatelet drug. Usually causes TTP within 2 weeks of starting. Median platelet count drops to 30,000/µL.
- Ticlopidine-older cousin of clopidogrel. Higher risk (1 in 1,600 users). Led to a black box warning and sales drop from $587 million to $82 million in just 3 years.
- Cyclosporine-used after organ transplants. Risk jumps to 1.5-15% if dose exceeds 5 mg/kg/day.
- Mitomycin C-a chemotherapy drug. Causes delayed, cumulative damage. Recovery can take months even after stopping.
Don’t overlook newer drugs either. TNF-alpha inhibitors like adalimumab (Humira) and checkpoint inhibitors like pembrolizumab (Keytruda) are now responsible for about 5-8% of new cases. These are often missed because they’re used for autoimmune diseases or cancer, where other causes of low platelets are already expected.
How Doctors Diagnose It
There’s no single blood test that confirms drug-induced TTP on its own. Diagnosis relies on three things:
- Clinical signs: Low platelets, signs of broken red blood cells (schistocytes, high LDH, low haptoglobin), and organ damage (brain, kidneys).
- Timing: Symptoms started within days or weeks of starting the drug-or returned after restarting it.
- Ruling out other causes: No signs of infection, no pregnancy, no genetic TTP, no other autoimmune disease.
ADAMTS13 enzyme activity below 10% confirms immune-mediated TTP. But you don’t wait for results. If the clinical picture fits, treatment starts immediately. Delaying plasma exchange by even 12 hours increases death risk.
What Happens If You’re Diagnosed
Once TTP is suspected, time is everything.
- Stop the drug immediately. No exceptions. Even if you think it’s unrelated.
- Start plasma exchange within 4-8 hours. This removes the bad antibodies and replaces them with healthy plasma. Daily sessions continue until platelets rise above 150,000/µL for two days straight.
- Use caplacizumab if available. This newer drug blocks clot formation and cuts recovery time by nearly 80% in immune cases. But it costs $18,500 per course and isn’t available everywhere.
- For dose-dependent cases (like cyclosporine): Plasma exchange doesn’t help much. Focus is on supportive care-kidney dialysis, blood transfusions, waiting for your blood vessels to heal.
Survival rates have improved since the 1990s, but they’re still grim: 10-20% die even with treatment. Why? Because diagnosis is often delayed. In Reddit patient forums and hospital records, 72% of people were first misdiagnosed. Many thought they had the flu. Others were told it was just low platelets from stress or infection.
What Patients and Families Should Watch For
If you’re taking any of these drugs, pay attention to these red flags:
- Sudden, unexplained bruising or tiny red dots on your skin (petechiae)
- Extreme fatigue that doesn’t go away
- Dark or tea-colored urine
- Confusion, headaches, slurred speech, or seizures
- Shortness of breath or chest pain without heart disease history
And if you’re on quinine-even in tonic water-stop it. A 2019 BMJ Case Report documented TTP in someone who drank two glasses of tonic water daily for three weeks. No prescription. No doctor’s note. Just a drink you buy at the grocery store.

Why This Is Getting Worse
The number of reported drug-induced TTP cases jumped 37% between 2015 and 2022. Why? Two big reasons:
- More people are taking high-risk drugs-especially biologics for autoimmune diseases and cancer.
- Doctors still don’t think of TTP fast enough. It’s not in most medical school curriculums. Emergency rooms aren’t trained to spot it.
Even the FDA’s own database shows quinine has an 18.7 times higher risk of causing TTP than other medications. Yet it’s still sold over the counter in tonic water, cough syrups, and leg cramp remedies.
How to Prevent It
Prevention is simple but often ignored:
- Always tell your doctor about every medication and supplement you take-including tonic water, herbal teas, and OTC pills.
- If you’re prescribed clopidogrel, ticlopidine, or cyclosporine, ask: “Could this cause TTP?”
- Don’t take quinine unless absolutely necessary-and never as a regular drink.
- Know the symptoms. If you develop sudden bruising, confusion, or fatigue after starting a new drug, go to the ER immediately.
There’s no cure for drug-induced TTP except stopping the drug and treating the damage. But with early action, most people recover fully. The key is recognizing it before your brain bleeds or your kidneys shut down.
What’s Next for TTP Treatment
Research is moving fast. Scientists are working on:
- Point-of-care ADAMTS13 tests that give results in under an hour (right now, it takes days).
- Genetic screening to find people at higher risk-like those with HLA-DRB1*11:01, who are 4.3 times more likely to get TTP from quinine.
- Better monitoring for new drugs during clinical trials, especially biologics and cancer therapies.
But until these tools are widely available, the best defense is awareness. If you’re on a medication that’s been linked to TTP, don’t assume it’s safe just because your doctor prescribed it. Ask questions. Know the signs. And if something feels wrong-trust your gut. It could save your life.

Andrew Short
January 17, 2026 AT 23:15Let me get this straight-you’re telling me people are dying because they drank tonic water? And doctors are too lazy to connect the dots? This isn’t medical negligence, this is criminal. Quinine has been around since the 1800s. If you’re still selling it in soda form without a goddamn warning label bigger than your face, you’re not a pharmaceutical company-you’re a death cult. Someone needs to sue the FDA into oblivion.