Metformin Side Effects: What You Need to Know About GI Issues and Lactic Acidosis
 Dec, 9 2025
Dec, 9 2025
Metformin Risk Assessment Tool
How This Tool Works
This tool estimates your risk of metformin-related side effects and lactic acidosis based on your health conditions and kidney function. It's not a substitute for professional medical advice, but helps you understand potential risks.
Metformin is the most common pill prescribed for type 2 diabetes. Millions of people take it every day. It works. It’s cheap. And for most, it’s safe. But not everyone tolerates it well. If you’ve started metformin and suddenly feel nauseous, have diarrhea, or feel unusually tired, you’re not alone. These aren’t rare side effects - they’re common. And while most fade with time, one rare but dangerous risk lurks in the background: lactic acidosis. Understanding both the everyday discomforts and the life-threatening risks can help you take metformin safely and stay in control of your health.
Why Your Stomach Feels Like It’s Revolting
About 1 in 3 people who start metformin get gastrointestinal side effects. That’s not a small number. It’s the norm. The most frequent complaints? Diarrhea, nausea, stomach pain, vomiting, and loss of appetite. These don’t show up after months - they hit fast. Most people notice them within the first week, and 7 out of 10 feel them in the first 30 days.It’s not your imagination. A 2021 review of nearly 7,500 patients showed that 53% of those with side effects had diarrhea. Nausea followed close behind at 28%. These aren’t mild. For some, they’re debilitating enough to make people quit the drug.
But here’s the good news: they usually go away. About 85% of people find relief within two to four weeks. Your body adapts. The key is patience - and strategy. Starting with a low dose helps. Many doctors now recommend beginning with 500 mg once a day, often with dinner. If you switch to the extended-release version (metformin ER), your chances of GI trouble drop by nearly half. One patient on Reddit, who’d been on metformin since 2008, said switching to 500 mg ER at night cut his diarrhea from 4-5 times a day to just occasional cramps in under 10 days.
Don’t crush the pills. Don’t take them on an empty stomach. Eat something - even a small snack - when you take your dose. Avoid high-fat meals. And if you’re still struggling after a month, talk to your doctor. There’s no shame in switching to a different formulation or trying another medication. Your comfort matters.
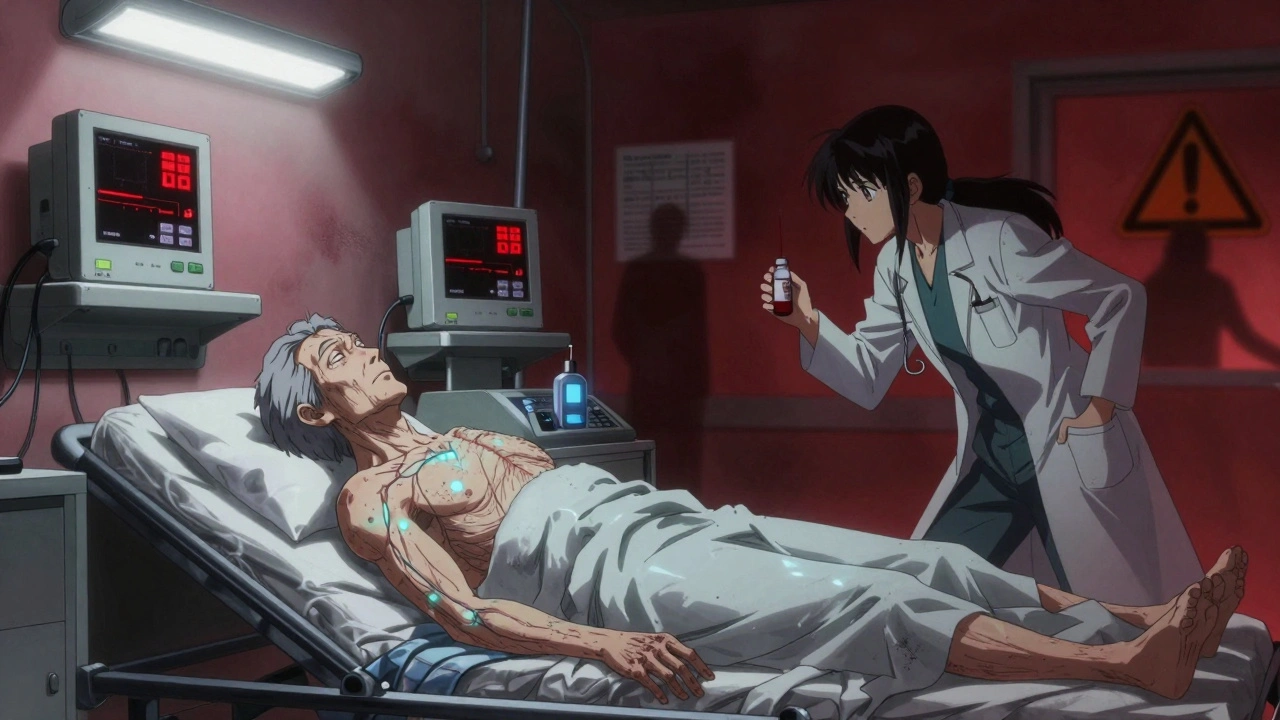
Lactic Acidosis: The Rare But Deadly Risk
When you hear the word “lactic acidosis,” it sounds scary. And it is. But you need to understand how rare it really is. The FDA put a black box warning on metformin in 1998 after 62 deaths were linked to it between 1959 and 1996. That scared a lot of people. But here’s what those numbers don’t tell you: in 2022, among 15.2 million metformin users in the U.S., only 12 confirmed cases of lactic acidosis were reported. That’s 0.079 cases per 100,000 people.That’s rarer than being struck by lightning. But when it happens, it’s serious. The death rate for confirmed cases is 30% to 50%. Why? Because metformin doesn’t just cause lactic acidosis - it makes it worse. It interferes with how your cells use oxygen, which causes lactate to build up. At the same time, it slows down your body’s ability to clear lactate. Two problems, one drug.
The symptoms don’t sneak up. They hit hard. Extreme fatigue. Rapid, shallow breathing. Nausea and vomiting. Abdominal pain. Muscle aches. Cold skin. If you feel this way, especially if you’ve been sick, dehydrated, or had a recent infection, don’t wait. Go to the ER. Time matters. Blood tests will check your pH, lactate level, and anion gap. If your pH is below 7.35 and lactate is above 5 mmol/L, you’re in danger.
Most cases aren’t caused by metformin alone. They’re caused by metformin plus something else - like kidney failure, liver disease, heart failure, or heavy alcohol use. In fact, 93% of cases happen in people with serious health problems. A 2020 study of over 1,200 cases found that severe kidney disease increases your risk by nearly 19 times. If your eGFR drops below 30, you’re not supposed to take metformin at all.
Who Should Not Take Metformin
Not everyone can take metformin. There are clear rules. The European Medicines Agency says you should stop if your creatinine is above 0.16 mmol/L in men or 0.13 mmol/L in women. That’s about 1.4 mg/dL and 1.1 mg/dL, respectively. Your doctor should check your kidney function every 3 to 6 months if your eGFR is between 45 and 59. If it’s below 45, they’ll check it monthly.If you’re scheduled for a CT scan or other imaging with contrast dye, you must stop metformin 48 hours before and not restart until 48 hours after. Contrast dye can stress your kidneys. If your kidneys can’t clear metformin during that time, lactate builds up fast.
Other red flags: liver disease, heart failure, recent heart attack, or drinking more than 3 alcoholic drinks a day. Alcohol and metformin are a dangerous mix. Together, they can trigger lactic acidosis even in people with normal kidneys.
Age matters too. People over 80 have nearly 5 times the risk. But age alone isn’t a reason to stop metformin. It’s the combination of age plus other health problems that raises the danger. As Dr. Kenneth Cusi from the University of Florida said, “The 50% mortality rate applies only to critically ill patients with multiple organ failures, not to stable outpatients.”
Myths and Misconceptions
There’s a lot of misinformation out there. Let’s clear it up.Myth: Metformin damages your kidneys.
Truth: It doesn’t. In fact, studies show it doesn’t increase the risk of kidney decline. If your kidneys are already failing, metformin can’t be cleared - but it’s not the cause.
Myth: Metformin causes dementia.
Truth: A 2021 study found no link. Some research even suggests it might protect brain health.
Myth: Metformin permanently lowers vitamin B12.
Truth: About 7% of long-term users do have lower B12 levels. But it’s reversible. The American Association of Clinical Endocrinologists now recommends checking B12 every year and supplementing if needed. No permanent damage.
Myth: Lactic acidosis is common.
Truth: It’s extremely rare when used correctly. The real risk is ignoring your health conditions while taking it.
What You Can Do Today
If you’re on metformin and feeling fine - great. Keep taking it. Don’t stop unless your doctor tells you to.If you’re having GI issues:
- Switch to extended-release metformin.
- Take it with food, not on an empty stomach.
- Start low, go slow. Don’t jump to 1,000 mg right away.
- Give it 4 weeks. Most side effects fade.
- If it doesn’t improve, talk to your doctor about alternatives.
If you’re at risk for lactic acidosis:
- Know your eGFR. Ask for it at every checkup.
- Stop metformin before any procedure with contrast dye.
- Avoid alcohol if you’re on metformin.
- Call your doctor immediately if you feel unusually tired, short of breath, or have unexplained stomach pain.
There’s a new metformin formulation approved in May 2023 - Metformin-ER-XR - that reduces GI side effects by over 40% in clinical trials. It’s not everywhere yet, but ask your pharmacist if it’s available.
Frequently Asked Questions
Can I take metformin if I have mild kidney problems?
Yes, but with caution. If your eGFR is between 30 and 45, your doctor may lower your dose and monitor you more closely. If your eGFR drops below 30, you should stop metformin. Regular kidney tests every 3-6 months are essential. Never assume your kidneys are fine - get them checked.
Does metformin cause weight loss?
Yes, modestly. Most people lose 2 to 4 kilograms (4 to 9 pounds) over the first year. It’s not a weight-loss drug, but it helps reduce appetite and may improve how your body uses insulin. That’s why it’s often preferred over other diabetes pills that cause weight gain.
How long do metformin side effects last?
For most people, gastrointestinal side effects fade within 2 to 4 weeks. About 85% of users see improvement by then. If symptoms persist beyond a month, talk to your doctor. You might need a lower dose, a different formulation, or a different medication.
Can I drink alcohol while taking metformin?
Occasional light drinking is usually okay, but heavy drinking is dangerous. More than 3 drinks a day increases your risk of lactic acidosis by nearly 7 times. Alcohol affects your liver and kidneys - the same organs that process metformin. Mixing them can be life-threatening.
Is metformin safe for older adults?
It can be, as long as kidney function is good. People over 80 have a higher risk of lactic acidosis - but only if they also have heart disease, infection, or dehydration. Many older adults take metformin safely for years. The key is regular kidney tests and avoiding dehydration, especially during illness.
What should I do if I miss a dose?
If you miss a dose, take it as soon as you remember - unless it’s almost time for your next one. Don’t double up. Missing one dose won’t cause blood sugar spikes right away, but consistently skipping doses reduces its effectiveness. Set a phone reminder if you need to.
What’s Next?
If you’re just starting metformin, give it time. Don’t quit because of stomach upset. Talk to your doctor about switching to extended-release. Eat with your pill. Start low. Wait it out.If you’ve been on it for years and feel fine, keep going. But don’t skip your kidney tests. Don’t ignore new symptoms like fatigue or breathing trouble. Don’t drink heavily. Don’t take it before a CT scan without telling your doctor.
Metformin isn’t perfect. But for most people, the benefits far outweigh the risks. The real danger isn’t the drug - it’s not knowing your limits. Stay informed. Stay checked. Stay alive.

Katherine Chan
December 11, 2025 AT 07:01Been on metformin for 3 years and honestly it saved my life
Yeah the stomach stuff was brutal at first but switched to ER and took it with dinner and boom no more drama
Don't quit too early you guys
Philippa Barraclough
December 11, 2025 AT 11:14The data on lactic acidosis is indeed reassuring when contextualized properly, though the black box warning remains a necessary precaution given the severity of outcomes in predisposed individuals
The incidence rate cited-0.079 per 100,000-is statistically negligible compared to other pharmaceutical risks, yet public perception remains skewed due to the dramatic nature of the condition and the historical context of its initial association with phenformin
It's also worth noting that many of the reported cases involve polypharmacy or undiagnosed renal impairment, which are confounding variables that should not be conflated with metformin monotherapy in healthy patients
Tim Tinh
December 11, 2025 AT 19:10lol i thought i was the only one who got the metformin belly
took it on empty stomach for a week and almost cried
switched to er with a peanut butter toast and now i’m fine
also i miss my doses all the time but my sugar’s still decent so maybe it’s chill
Olivia Portier
December 13, 2025 AT 05:00For anyone scared of the GI stuff-just start at 500mg once a day and don’t rush it
I was terrified at first but my doc told me to think of it like training for a marathon-you don’t run 10 miles day one
Now I’m on 1500mg ER and feel great
And yes, the B12 thing is real-I started taking a supplement and my energy came back
You’re not broken, you’re just adjusting
Asset Finance Komrade
December 13, 2025 AT 21:51Metformin is not a miracle drug-it is a pharmaceutical compromise born of economic necessity and institutional inertia
The fact that it remains first-line despite its gastrointestinal toxicity suggests systemic prioritization of cost over comfort
And while lactic acidosis is statistically rare, the risk-benefit calculus shifts dramatically in populations with comorbidities-yet screening remains inconsistent
One must ask: is this drug truly safe, or merely tolerated by those with no alternatives?
Jennifer Blandford
December 14, 2025 AT 10:30I cried the first week on metformin like I lost my dog
But then I started taking it with my 10pm snack and now I forget I’m even on it
Also my jeans fit better and I didn’t even try
PS: my doc said I’m a walking miracle and I believe her
Brianna Black
December 15, 2025 AT 16:21The misinformation around metformin is alarming. Many patients believe it causes kidney damage, when in fact, it is one of the safest antihyperglycemic agents available when used appropriately
Regular monitoring of eGFR is non-negotiable, and the 48-hour hold before contrast imaging is a standard of care that must be enforced
Patients must be educated-not frightened. Knowledge is the most effective prophylaxis against adverse outcomes
Shubham Mathur
December 17, 2025 AT 00:04Stop whining about stomach issues you’re all weak
My grandma took metformin for 20 years and never complained
And you’re crying about diarrhea like it’s the end of the world
Also check your kidneys before blaming the drug
And yes alcohol is poison with this med-stop drinking if you want to live
Stacy Tolbert
December 18, 2025 AT 16:50I stopped metformin because I felt like I was dying
Not from diabetes-from the pill
My stomach hurt every day and I lost 15 lbs in a month
I didn’t want to be a skeleton
My doctor said it was normal but I just couldn’t do it anymore
Now I’m on GLP-1 and I feel human again
It’s not about being strong-it’s about being alive
Iris Carmen
December 19, 2025 AT 05:52metformin er is a game changer honestly
no more midday runs to the bathroom
took me 3 weeks to figure it out but now i’m chill
also i take my pill with a banana and it’s magic