Opioids and Sleep Apnea: How Opioids Trigger Dangerous Breathing Problems During Sleep
 Nov, 28 2025
Nov, 28 2025
Opioid Sleep Apnea Risk Calculator
Opioids can suppress breathing during sleep, leading to dangerous pauses in breathing. This tool estimates your risk based on dosage and health factors. High-risk users should consult a doctor immediately.
Your Risk Assessment
When you take opioids for pain, you might not think about your breathing-especially while sleeping. But for many people, that’s exactly when things go wrong. Opioids don’t just dull pain; they quietly shut down the parts of your brain that keep you breathing steadily through the night. This isn’t rare. Around 30-40% of people on long-term opioid therapy develop serious sleep-related breathing problems, and for some, it’s deadly.
What Happens When Opioids Meet Your Breathing System
Your brain has a built-in system that keeps you breathing, even when you’re asleep. It monitors carbon dioxide levels, adjusts your breathing rate, and keeps your airway open. Opioids mess with this system at multiple levels. They hit specific receptors in the brainstem-especially in the parabrachial complex and the pre-Bötzinger complex-areas that control how fast and how deeply you breathe. The result? Slower, shallower breaths. Exhalations get longer. Sometimes, you stop breathing entirely for 10, 20, even 40 seconds at a time. This isn’t just snoring. It’s central sleep apnea: your brain literally forgets to tell your lungs to breathe. Studies show that people on high-dose opioids (100 morphine milligram equivalents or more daily) average over 15 breathing pauses per hour. For someone without opioids, that number is usually under 5.Why Sleep Makes It Worse
Sleep isn’t just rest-it’s a vulnerability window for opioid users. When you fall asleep, your body naturally reduces its drive to breathe. That’s normal. But opioids amplify this drop. Without the wakefulness signal to keep breathing steady, your brain’s respiratory control slips into a dangerous lull. Add to that the fact that opioids weaken the muscles that hold your airway open. The genioglossus, the main tongue muscle that prevents your airway from collapsing, loses up to 60% of its activity under opioid influence. So you’re not just having central apnea-you might also be getting obstructive apnea. It’s a double hit: your brain stops sending the signal to breathe, and your throat physically closes off.The Real Danger: Silent Oxygen Drops
Many people don’t realize they’re in trouble because their oxygen levels don’t crash right away. Your body compensates at first-breathing harder when awake, increasing heart rate. But during sleep, these tricks fail. By the time your pulse oximeter shows low oxygen, you’ve already been in danger for minutes. This is why so many opioid-related deaths happen at night. People wake up gasping, or worse-they don’t wake up at all. In 2021, over 80,000 Americans died from opioid overdoses, and respiratory depression was the cause in about 70% of those cases. Most of those deaths occurred during sleep, often without witnesses.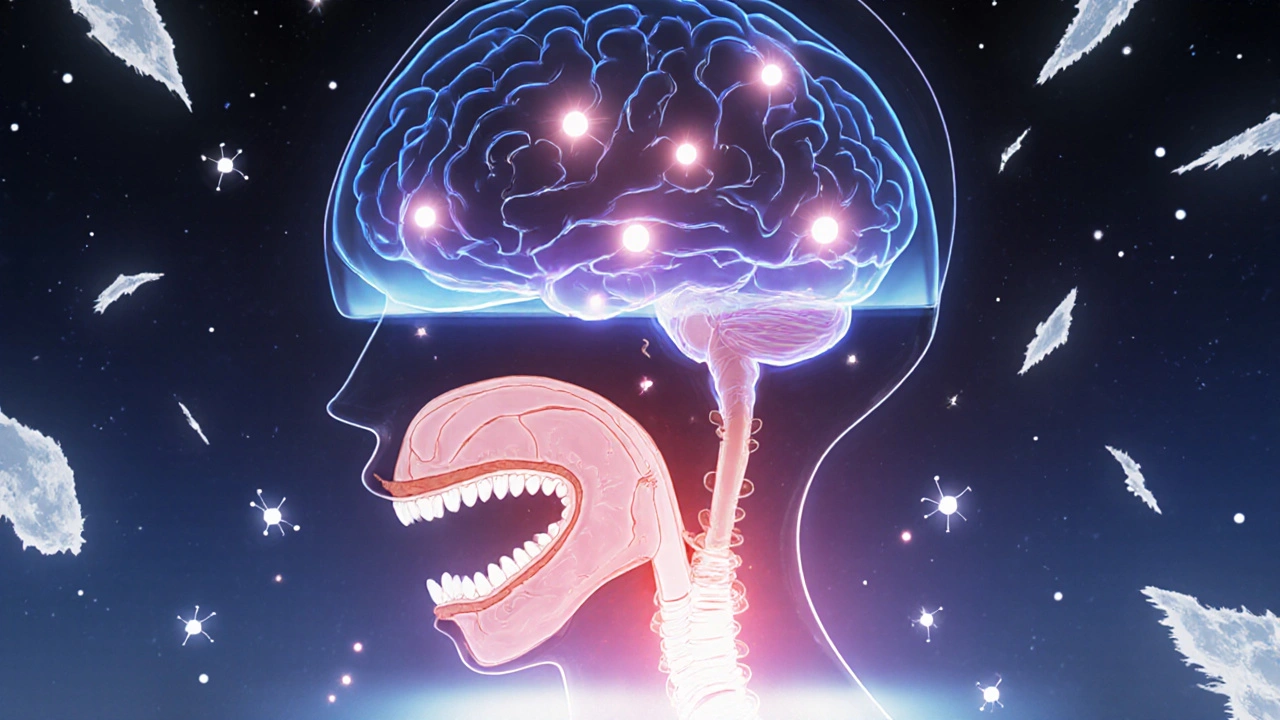
Who’s Most at Risk?
Not everyone on opioids develops sleep apnea. But some groups are far more vulnerable:- People with existing sleep apnea before starting opioids
- Those taking 100+ morphine milligram equivalents per day
- Anyone combining opioids with benzodiazepines, alcohol, or sleep aids
- Individuals with obesity, heart failure, or COPD
- People with genetic variants in the OPRM1 gene, which affects how opioids bind to brain receptors
What Clinicians Should Be Doing
Doctors often miss this. Only 15-20% of primary care providers routinely screen chronic opioid users for sleep apnea. That’s alarming, given that the American Society of Anesthesiologists recommends baseline sleep studies for anyone on long-term opioid therapy. If you’re on opioids and feel exhausted during the day, have morning headaches, or wake up gasping for air, ask for a sleep study. A home sleep apnea test can detect central apnea patterns that standard overnight monitoring might miss. And if you’re on high doses or taking other sedatives, your doctor should consider naloxone at home-not just as an emergency tool, but as a safety net.
What You Can Do Right Now
If you or someone you know is on opioids:- Don’t combine opioids with alcohol, benzodiazepines, or sleeping pills. The risk of fatal breathing depression jumps by 300-500%.
- Watch for signs: excessive daytime sleepiness, loud snoring, waking up choking, unrefreshing sleep.
- Ask your doctor for a sleep apnea screening-even if you don’t think you’re at risk.
- Keep naloxone on hand if you’re on high doses or live alone. It can reverse an overdose in minutes.
- Consider non-opioid pain management options. Physical therapy, nerve blocks, or certain antidepressants can help without risking your breathing.
The Future: Safer Opioids and Personalized Medicine
Researchers are working on opioids that relieve pain without shutting down breathing. New compounds, called MOR-biased agonists, are showing promise in early trials. In animal studies, they deliver 70-80% of the pain relief of traditional opioids but cause only 20-30% of the respiratory depression. Genetic testing is also on the horizon. Within five years, doctors may screen for OPRM1 gene variants to predict who’s at highest risk for opioid-induced respiratory depression. That could mean personalized dosing-or avoiding opioids altogether for some patients. For now, the safest approach is simple: treat opioids like a powerful tool that demands respect. They’re not harmless. They don’t just affect your pain-they affect your breath. And in sleep, that’s when the silence can kill.Can opioids cause sleep apnea even if I didn’t have it before?
Yes. Opioids can trigger central sleep apnea in people with no prior history. They suppress the brain’s breathing control centers, leading to pauses in breathing during sleep. Studies show 30-40% of long-term opioid users develop clinically significant sleep-disordered breathing, even if they were healthy sleepers before starting treatment.
Is sleep apnea from opioids reversible?
Often, yes. When opioids are reduced or stopped, breathing patterns usually improve within days to weeks. However, if the apnea has been severe and prolonged, some damage to the brain’s respiratory control system may linger. Early intervention improves outcomes. Using CPAP or other breathing support during treatment can help protect your lungs while you taper off.
Can naloxone prevent opioid-induced sleep apnea?
Naloxone doesn’t prevent sleep apnea-it reverses it after it happens. It blocks opioid receptors in the brainstem, restoring breathing within minutes. It’s not a daily preventive tool, but having it on hand can be lifesaving if someone stops breathing during sleep. It’s recommended for anyone on high-dose opioids, especially those living alone.
Why don’t pulse oximeters always catch opioid-related breathing problems?
Pulse oximeters measure oxygen levels, not breathing effort. In the early stages of opioid-induced respiratory depression, your body may compensate by increasing heart rate or breathing deeper between pauses. Oxygen levels stay normal until you’ve had multiple prolonged breath holds. By the time oxygen drops, you’re already in critical danger. Capnography (measuring carbon dioxide) is a better early warning tool, but it’s rarely used outside hospitals.
Are there alternatives to opioids for chronic pain that don’t affect breathing?
Yes. For many types of chronic pain, non-opioid options like physical therapy, cognitive behavioral therapy, certain antidepressants (like duloxetine), nerve blocks, or anti-seizure medications (like gabapentin) can be effective without suppressing breathing. Even low-dose NSAIDs or topical treatments can help. The key is working with a pain specialist to find a combination that works for you-without risking your life.

Phil Thornton
November 30, 2025 AT 03:46Opioids and sleep apnea? Yeah, I knew someone who stopped breathing in his sleep after a back surgery. They found him blue. No one knew he was on pain meds.
Pranab Daulagupu
November 30, 2025 AT 09:00Central apnea from opioids is underdiagnosed because it doesn’t show up on standard sleep studies. Capnography’s the gold standard, but most home tests don’t even measure CO2. We’re flying blind.
Barbara McClelland
December 1, 2025 AT 07:40If you’re on opioids and feel like you’re never rested, don’t brush it off as ‘just aging.’ Get tested. Seriously. Your breath matters more than you think.
Alexander Levin
December 1, 2025 AT 10:58Big Pharma knows this. They just don’t care. Why? Because naloxone is a cash cow. 😒
Ady Young
December 2, 2025 AT 06:28I’ve seen this in my clinic. A guy on 120 mg MME, no prior apnea, started snoring like a chainsaw. Sleep study confirmed central apnea. Tapered him off, breathing normalized in 3 weeks. It’s real.
Travis Freeman
December 2, 2025 AT 16:03My uncle in rural Kentucky was on oxycodone for 7 years. Never knew he had breathing issues till he passed in his sleep. No warning. No one knew. This needs more awareness.
Sean Slevin
December 3, 2025 AT 18:50...and yet, we still prescribe opioids like they’re Advil... I mean, seriously... do we even remember what the brainstem does?... It’s not just pain... it’s survival... and we’re gambling with it... every single time...
Chris Taylor
December 5, 2025 AT 03:24My mom’s on tramadol for fibro. She wakes up gasping sometimes. I made her ask her doc about a sleep study. She said no, but I’m gonna push. This isn’t normal.
Melissa Michaels
December 5, 2025 AT 04:14It is imperative that clinicians initiate screening protocols for sleep-disordered breathing in all patients prescribed long-term opioid therapy. The evidence is unequivocal.
Chetan Chauhan
December 6, 2025 AT 02:34Wait so you're saying opioids make you stop breathing... but i heard they help you sleep better? lol maybe i read wrong
Nathan Brown
December 7, 2025 AT 11:38It’s not just about the drugs-it’s about how we treat pain in America. We reach for the quick fix instead of the hard work. Physical therapy takes time. Naloxone is a Band-Aid on a bullet wound.
Matthew Stanford
December 9, 2025 AT 04:14My cousin’s a nurse in Oregon. She says they’ve started giving out naloxone kits with every opioid script now. Small step. But it’s something.
Olivia Currie
December 10, 2025 AT 07:13Imagine being asleep... and your own body forgets to breathe... and no one hears you... no one knows... and then... silence. This isn't just medical-it's a tragedy waiting to happen in every home.
Curtis Ryan
December 11, 2025 AT 07:33My cousin got off opioids after this. Now he does yoga and acupuncture. He says he sleeps better than ever. No more nightmares. No more gasping. Just peace.
Rajiv Vyas
December 12, 2025 AT 11:10They say opioids cause apnea but what if it’s the sleep study machines themselves? I heard they use fake CO2 sensors... part of the surveillance grid...