Out-of-Pocket Costs: What Patients Pay for Generics vs Brand-Name Drugs
 Dec, 22 2025
Dec, 22 2025
When you pick up a prescription, the price on the receipt can feel random. One month, your generic blood pressure pill costs $4. The next, it’s $18. Meanwhile, your neighbor’s brand-name version of the same drug is only $12. Why? It’s not about quality. It’s not about effectiveness. It’s about how the system is built-and who’s paying for it.
Generics aren’t cheaper because they’re worse
The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also prove they work the same way in the body. That’s not a guess. It’s science. So if your doctor prescribes lisinopril and you get the generic, you’re getting the exact same medicine your body needs. The only differences? The shape, color, or filler ingredients-things that don’t affect how the drug works. Yet, generics cost 80 to 85% less than their brand-name equivalents. In the U.S., about 90% of all prescriptions filled are for generics. But here’s the twist: even though they make up most of the prescriptions, they only account for about 18% of total drug spending. That’s because brand-name drugs, though rarely prescribed, are priced so high they drag up the total cost.Insurance design decides what you pay
Your out-of-pocket cost doesn’t just depend on the drug’s list price. It depends on your insurance plan. There are three main ways plans charge you:- Copay: A flat fee, like $5 or $15, no matter what the drug costs.
- Coinsurance: A percentage of the drug’s price, like 20%.
- Deductible: You pay 100% until you hit a certain amount.
The Medicare Part D trap
Medicare Part D has a strange loophole that makes some generics cost more than brand-name drugs. It’s called the “donut hole,” or coverage gap. Here’s how it works: Once you and your plan have spent a certain amount on drugs, you enter the gap. You pay a higher share until you hit the catastrophic coverage threshold. At that point, you only pay 5% of the drug’s cost. But here’s the catch: Brand-name drug manufacturers are required to give a discount during the gap-and that discount counts toward your out-of-pocket spending. Generic manufacturers? They don’t have to. So if you’re taking a high-priced generic, you have to spend way more before you reach catastrophic coverage. In 2019, a brand-name drug user needed to spend $982 to get out of the gap. A generic drug user? $3,730. That’s nearly four times more. Even though the generic cost less per pill, the system made you pay more to get the same relief.
When paying cash beats insurance
You might think insurance always saves you money. But for generics, that’s not always true. A 2024 study found that 11.8% of generic prescriptions cost less when paid in cash through services like Mark Cuban Cost Plus Drug Company. On average, people saved $4.96 per prescription. For uninsured patients, the savings were even bigger. Medicaid patients didn’t save much-because their plans already had low copays. Why? Because insurance pricing is hidden. Pharmacies and pharmacy benefit managers (PBMs) negotiate secret deals. The price you see on your bill isn’t the real cost. It’s a middleman’s markup. Cash-only pharmacies cut out the middlemen. They charge a transparent cost plus a small fee. No rebates. No hidden contracts. Just the real price. In 2020, only 4% of U.S. prescriptions were paid in cash. But 97% of those cash payments were for generics. That tells you something: people are figuring out how to game the system.Doctors can block generics-even if you want them
Your doctor can write “dispense as written” or “do not substitute” on your prescription. That means the pharmacist can’t give you the generic, even if it’s cheaper. Sometimes, this is medically necessary. Other times, it’s just habit-or because the drug company paid the doctor to promote the brand. If you’re on a high-deductible plan and your doctor prescribes a brand-name drug, ask: “Is there a generic?” If they say no, ask why. If they can’t give you a clear medical reason, you might be paying more than you need to.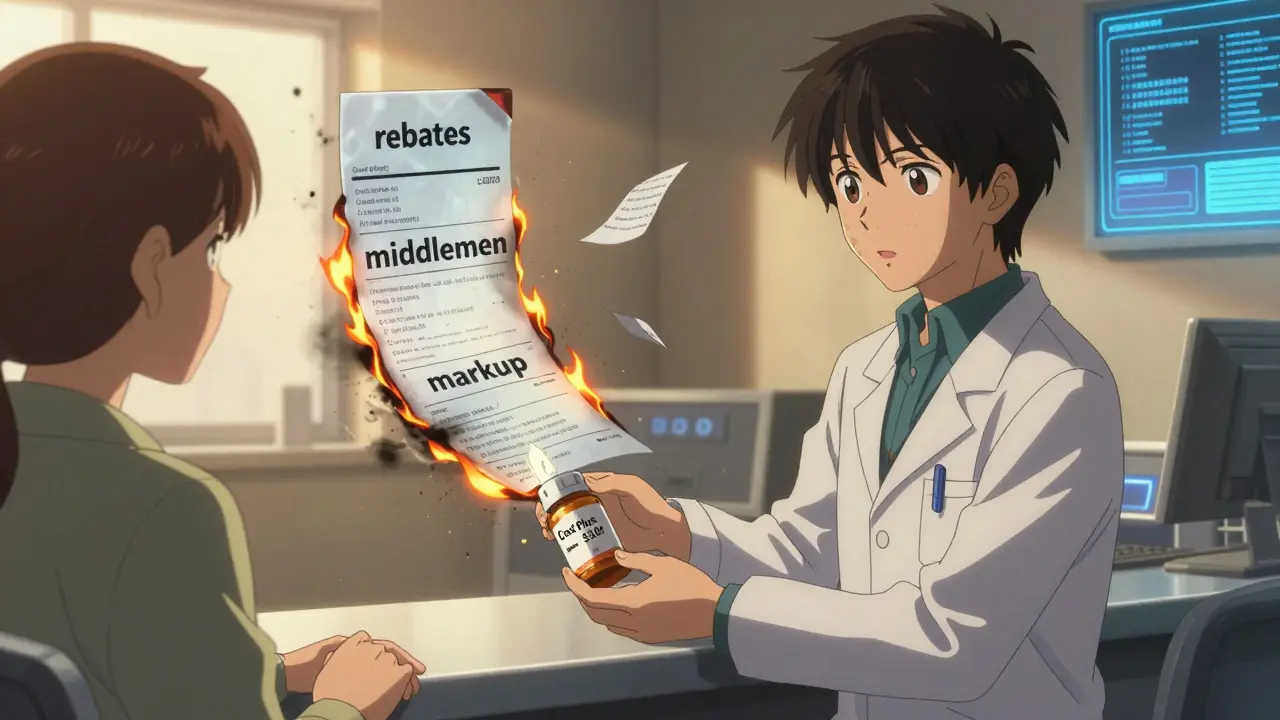
Why the system is broken
The U.S. spends $350 billion a year on prescription drugs. Generics saved $338 billion in 2020 alone. That’s more than the entire annual budget of many states. But the savings aren’t reaching patients. Why? Because the system rewards complexity. PBMs and insurers profit from opaque pricing. Drug manufacturers raise list prices to boost rebates-rebates that go to insurers, not patients. The result? Patients pay more for the same medicine, even when generics are available. Dr. Stacie Dusetzina from Vanderbilt University put it simply: “The system makes brand-name drugs cheaper to use than generics-not because they’re better, but because of how the rules are written.”What you can do right now
You don’t have to accept whatever price you’re given. Here’s what works:- Always ask if a generic is available-even if your doctor prescribes a brand.
- Check GoodRx or Cost Plus Drug Company before filling your prescription. Sometimes, cash price beats insurance.
- If you’re on Medicare Part D and take high-cost generics, track your out-of-pocket spending. You might be stuck in the donut hole longer than you need to be.
- Call your pharmacy. Ask: “What’s the cash price?” Then ask: “What’s my copay?” Compare.
- If you’re paying more than $20 for a common generic like metoprolol or omeprazole, you’re likely being overcharged.

Austin LeBlanc
December 24, 2025 AT 04:50Bro, I paid $23 for metoprolol last week. Same pill, same pharmacy. This week? $5. I called them. They said my insurance ‘re-negotiated’ the price. LMAO. No one knows what’s going on. I just pay cash now. Save my ass every time.
Also, my grandma takes 7 generics. She’s on Medicare. She’s in the donut hole like it’s a damn timeshare. She cried last month because she had to choose between her blood pressure pill and insulin. This system is cruel.
And don’t get me started on PBMs. They’re middlemen who don’t make drugs. They just shuffle numbers around and get rich. We’re the ones getting screwed.
Someone needs to burn it all down.
PS: GoodRx saved me $112 last month. Use it. It’s free.
niharika hardikar
December 25, 2025 AT 14:42The structural inefficiencies inherent in the pharmaceutical supply chain are exacerbated by the absence of price transparency mechanisms and the perverse incentives embedded within pharmacy benefit manager (PBM) reimbursement models. The phenomenon wherein generic medications, despite therapeutic equivalence, are subject to elevated out-of-pocket expenditures due to Medicare Part D’s coverage gap architecture constitutes a clear case of regulatory failure.
Furthermore, the absence of mandatory manufacturer rebates for generic drugs during the donut hole phase represents a profound inequity in policy design, disproportionately burdening low-income beneficiaries who rely on cost-effective therapeutics. A policy intervention mandating parity in out-of-pocket accumulation thresholds is both ethically imperative and fiscally prudent.
EMMANUEL EMEKAOGBOR
December 27, 2025 AT 01:35Man, this is wild. I’m from Nigeria, and here, generics are the only option. We don’t even have brand names most of the time. And the prices? Like $0.20 for blood pressure pills. I came to the US for school and I nearly fainted at the pharmacy counter.
It’s not about the drug. It’s about who controls the money. The system here feels like a casino where the house always wins, and the patient is the sucker.
But hey, at least you guys have options. We just pray the medicine doesn’t run out.
Still… I’m glad someone’s talking about this. Maybe change can come.
CHETAN MANDLECHA
December 27, 2025 AT 10:05So I asked my doc for a generic for my statin. He said ‘no’ - said it was ‘not equivalent.’ I asked for the study. He said ‘I just know.’
So I went to the pharmacy, asked for the cash price. $4.50. Insurance copay? $38.
I paid cash. Walked out. Didn’t say a word to the doctor. He’ll find out next month when my refill comes in.
Also - why do doctors still write ‘do not substitute’ like it’s 2005? The FDA doesn’t even care anymore.
Ajay Sangani
December 27, 2025 AT 22:49it’s weird how we think medicine is about health but its really about money and contracts and who gets what cut. like the pill is the same but the system makes one cost 10x. its like buying water but the bottle you get it in decides the price. why does the shape of the pill matter? it doesnt. but the system says it does.
also i think the donut hole thing is just a scam. they made it so complicated on purpose so people give up. i read about it and i still dont get it. and im not dumb.
we need to stop trusting doctors to fix this. they’re stuck in the same system. we need to fix it ourselves. cash. goodrx. ask. ask again. dont be shy.
Gray Dedoiko
December 28, 2025 AT 11:05I used to think insurance was helping me. Then I got a $120 bill for a $3 generic. I called my insurer. They said, ‘Oh, you’re on coinsurance.’ I didn’t even know what that meant.
I switched to cash for all my generics. Now I pay $5 a month. I’m not rich. I’m just tired of being played.
Also - if your doctor says ‘no generic,’ ask why. If they say ‘because it’s better’ - they’re lying. Ask for the data. Most won’t have it.
Thanks for posting this. I’ve been screaming into the void about this for years.
Joe Jeter
December 29, 2025 AT 02:52Let me guess - you think the problem is ‘big pharma’? Nah. It’s the government. They created this mess by letting PBMs negotiate secret rebates, then pretending they’re saving patients. The FDA approves generics, sure - but they don’t regulate pricing. That’s not a flaw. That’s the design.
And you think paying cash is ‘gaming the system’? No. You’re just avoiding the rigged game. The system is designed to make you think insurance is saving you. It’s not. It’s extracting more.
Also - ‘generics saved $338 billion’? Who cares? That money didn’t go to you. It went to insurers and PBMs. You’re still paying $25 for lisinopril. That’s not a win. That’s theft dressed up as savings.
Sidra Khan
December 29, 2025 AT 17:41OMG I just realized I’ve been overpaying for my omeprazole for 3 years. 😭
I’m crying. Not because I’m emotional - because I’m mad. Why didn’t anyone tell me? Why did I trust my insurance? Why did I think ‘copay’ meant ‘fixed price’?
Just went to GoodRx. Cash price: $4. Insurance copay: $28. I’m switching tomorrow.
Also - why does my doctor still write ‘dispense as written’? Is he getting kickbacks? I’m gonna ask next time. I’m done being a sucker.
Lu Jelonek
December 31, 2025 AT 14:12I work as a pharmacist in rural Ohio. I see this every day. People come in with prescriptions for brand-name drugs, confused why they’re paying $80 when the generic is $3.
I tell them. They’re shocked. Sometimes they cry.
But here’s the thing - I can’t override the doctor’s ‘do not substitute’ note. Even if I know it’s unnecessary. Even if I know the patient can’t afford it. I’m bound by the script.
It’s not the pharmacy’s fault. It’s not the doctor’s fault. It’s the system. And we’re all just trying to survive inside it.
Ask for cash prices. Always. Even if you have insurance. It’s your right.
Ademola Madehin
January 1, 2026 AT 05:22YOOOOO I JUST FOUND OUT I WAS PAYING $45 FOR LIPITOR WHEN I COULD’VE PAID $5 FOR ATORVASTATIN??
I’M SCREAMING RIGHT NOW. MY MOM’S MEDS COST MORE THAN MY RENT.
WHY IS THIS A THING?? WHY DOESN’T THE GOVERNMENT DO SOMETHING??
I JUST WENT TO COST PLUS DRUG CO. I BOUGHT 3 MONTHS OF MY DAD’S BLOOD PRESSURE PILLS FOR $18.
WE’RE ALL BEING ROBBED. AND NO ONE TALKS ABOUT IT.
EVERYONE WHO READS THIS - GO CHECK YOUR PRESCRIPTIONS RIGHT NOW. DON’T WAIT. I’M STILL SHAKING.
suhani mathur
January 2, 2026 AT 07:19Oh wow, so the donut hole is a trap for people who take generics? That’s not a loophole - that’s a death sentence for low-income seniors.
And you know what’s funny? The same people who scream about ‘socialized medicine’ are the ones who benefit the most from this broken system. They get brand-name drugs with copays so low they don’t even notice.
Meanwhile, my cousin in Alabama pays $180/month for her generics because her plan doesn’t count them toward the gap.
It’s not about drugs. It’s about who gets to live.
And we’re all just waiting for someone to fix it.
...Or we fix it ourselves. GoodRx. Cash. Ask. Repeat.
Bartholomew Henry Allen
January 3, 2026 AT 15:09The FDA regulates safety. Not pricing. That is the truth. The system is not broken. It is working exactly as designed. PBMs, insurers, and manufacturers profit from complexity. Patients are collateral. This is not an accident. It is policy.
Stop blaming doctors. Stop blaming pharmacists. They are cogs. The machine is the problem.
Pay cash. Use GoodRx. Demand transparency. Do not rely on insurance. Insurance is not your friend. It is a middleman with a monopoly.
And if you are on Medicare Part D - you are being exploited. Period.