Patient Counseling on Generics: What Pharmacists Must Discuss to Improve Adherence and Trust
 Dec, 10 2025
Dec, 10 2025
When a patient picks up a prescription and sees a pill that looks completely different from what they’ve been taking, it’s natural to feel confused-or even worried. Generic medication isn’t a lesser version. It’s the same active ingredient, same effectiveness, same safety profile. But without clear explanation from the pharmacist, that difference in color, shape, or size can lead patients to stop taking their medicine altogether.
Why Generic Counseling Isn’t Optional
Federal law under OBRA ’90 made it clear: pharmacists must counsel patients on every new or refilled prescription. This isn’t a suggestion. It’s a legal requirement in all 50 states. And when it comes to generics, the stakes are higher. A 2023 Consumer Reports survey found that 43% of patients believe generic drugs are less effective. Another 37% think they cause more side effects. These aren’t just myths-they’re barriers to health. The truth? Generics are bioequivalent. That means they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. The FDA requires this. But patients don’t know that unless someone tells them.What Pharmacists Must Say-The 5 Essential Points
Generic counseling isn’t about reading from a script. It’s about answering the unspoken questions patients are too embarrassed or rushed to ask. Here’s what needs to be covered every time a generic is dispensed:- Confirm the patient’s identity. Always start here. Make sure you’re talking to the right person. This isn’t just protocol-it’s safety.
- Explain why the change happened. Say clearly: "Your insurance or state law requires us to dispense the generic version. It’s not a mistake. It’s standard practice."
- Describe the physical differences. Show them. "This pill is white and oval instead of blue and round. That’s because the inactive ingredients-like dyes and fillers-are different. The medicine inside is exactly the same."
- Reaffirm bioequivalence and safety. Use plain language: "The FDA tests these generics to make sure they work just like the brand. Thousands of patients take them safely every day."
- Verify understanding with the teach-back method. Don’t just ask, "Do you have any questions?" Ask: "Can you tell me how you’ll take this pill and why it’s the same as your old one?" If they can’t explain it, you haven’t finished counseling.
The Cost of Silence
One Reddit user shared: "I stopped my blood pressure meds for two weeks because the pills looked different. I thought the pharmacy gave me the wrong thing." That’s not rare. In fact, studies show that 68% of patients who received clear generic counseling felt more confident in their medication-compared to just 32% who didn’t. Pharmacists aren’t just dispensing pills. They’re preventing hospitalizations. When patients stop taking meds because they don’t understand the switch, it leads to worse outcomes: higher blood pressure, uncontrolled diabetes, more ER visits. The cost? Billions in avoidable healthcare spending each year.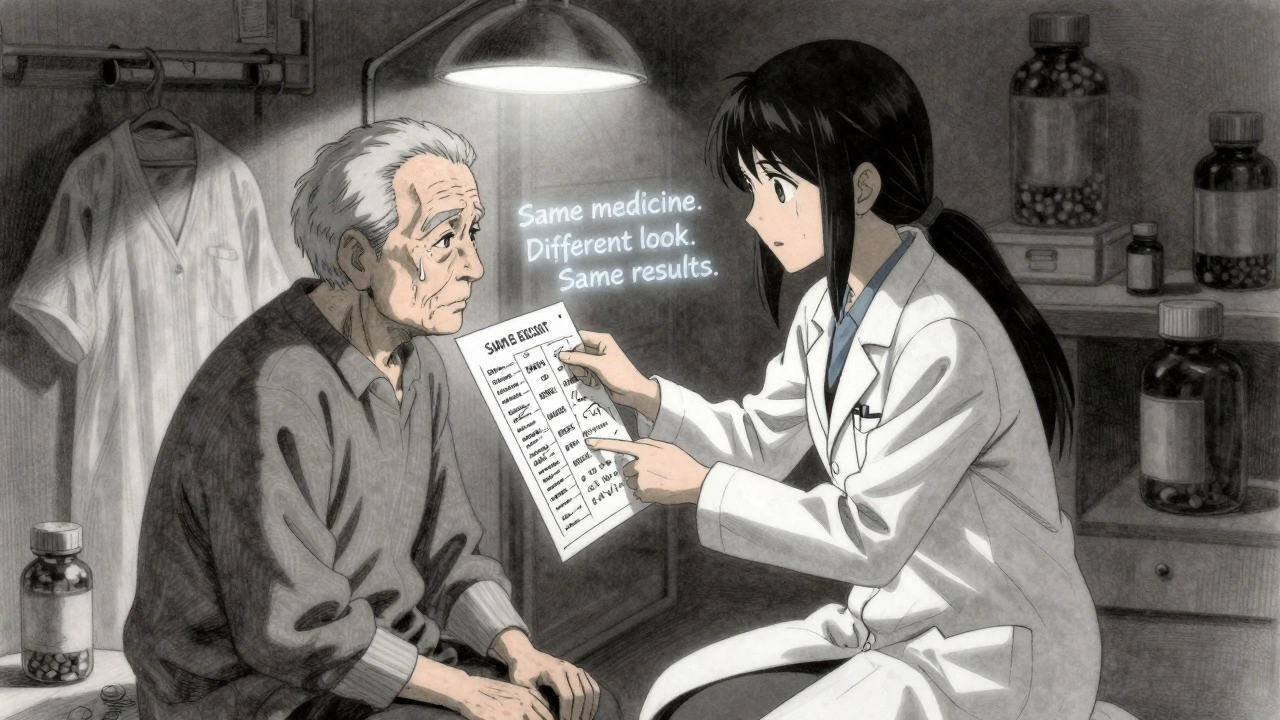
State Laws Vary-But the Standard Shouldn’t
Forty-nine states allow pharmacists to substitute generics automatically. But only 32 require them to tell the patient. In 17 states, you only need to explain if the patient asks. That creates a dangerous gap. In California, pharmacists must check a box on the record confirming they discussed the substitution. In Texas, they just note "counseling offered." That inconsistency means a patient’s experience depends on where they live-not on what’s best for their health. The best practice? Don’t wait for the law to catch up. Counsel every time. It’s the ethical thing to do. And it’s what patients expect. Gallup surveys show patient demand for clear generic explanations has risen 37% since 2018.Time Is Short-But You Can Still Do It Right
The average pharmacist spends just 1.2 minutes per patient on counseling. That’s not enough to explain complex drug interactions. But it’s more than enough to cover the five points above. Here’s how to make it fast and effective:- Use visual aids. Keep a printed chart showing brand vs. generic pill images for common medications.
- Keep a one-page handout ready. Simple language: "Same medicine. Different look. Same results."
- Train technicians to say: "The pharmacist will explain your new pills when you pick them up." Never let them deliver the counseling.
- Use tech tools. Most major pharmacy chains now use electronic prompts that pop up when a generic is dispensed-reminding you to cover key points.

What Patients Really Think
Patient reviews on Trustpilot reveal a pattern: 57% of negative feedback mentions feeling "rushed" during the generic explanation. Meanwhile, positive reviews often say: "My pharmacist took two minutes to show me the difference. That made all the difference." One patient wrote: "I thought the generic wasn’t working because my migraines came back. Turns out, I was taking it wrong. My pharmacist showed me the timing-right after breakfast, not before bed. That one conversation saved me months of pain." That’s the power of counseling. It’s not about filling out forms. It’s about connecting.What’s Changing in 2025
CMS updated its guidance in early 2024: now, pharmacists must document what was discussed-not just that counseling happened. That means writing down things like "explained bioequivalence," "addressed concern about pill color," or "confirmed patient understands same active ingredient." The National Association of Boards of Pharmacy is testing a standardized checklist across 12 states. Early results show a 28% jump in patient understanding when pharmacists use it. By 2026, AI tools will likely flag patients with a history of stopping generics based on prescription patterns or demographic data. That means pharmacists won’t guess who needs extra help-they’ll know.Final Thought: Your Role Is Bigger Than You Think
You’re not just the person who hands out pills. You’re the last line of defense against misunderstanding, non-adherence, and preventable harm. When a patient walks away confused about their generic medication, the problem isn’t the drug. It’s the conversation that never happened. Make that conversation count. Use the five-point framework. Show them the pill. Say it plainly. Ask them to repeat it back. Document it clearly. Because in the end, it’s not about generics versus brand. It’s about trust. And trust is built one honest conversation at a time.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent-meaning they deliver the same amount of medicine into the bloodstream at the same rate. Thousands of studies confirm this. Generic drugs are not "weaker" or "slower." They’re the same medicine, often at a fraction of the cost.
Why do generic pills look different from brand-name ones?
The difference in color, shape, or size comes from inactive ingredients-like dyes, fillers, or coatings. These don’t affect how the medicine works. Federal law requires generics to look different from brand-name drugs to avoid confusion and trademark infringement. That’s why your pill might be white and oval instead of blue and round. But the active ingredient inside is identical.
Can pharmacists substitute generics without telling me?
In 17 states, pharmacists can substitute generics without notifying you unless you ask. But in 32 states, they’re required to tell you before making the switch. Even if your state doesn’t require it, the best practice is to always explain the change. Many patients assume a different-looking pill is a mistake-or worse, a counterfeit. Clear communication prevents dangerous misunderstandings.
What should I do if I think my generic isn’t working?
Don’t stop taking it. Call your pharmacist. Many times, the issue isn’t the drug-it’s how or when you’re taking it. Maybe you’re skipping doses, taking it with food when you shouldn’t, or confusing it with another pill. Your pharmacist can review your routine, check for interactions, and confirm the medication is correct. Rarely, a patient may have a sensitivity to an inactive ingredient-but that’s uncommon and can be addressed by switching to another generic version.
Is counseling required every time I refill a generic prescription?
Yes. Federal law and state regulations require pharmacists to offer counseling every time a prescription is filled or refilled. Even if you’ve taken the same generic for years, the law still applies. Changes in your health, other medications, or even the manufacturer of the generic can affect how you use it. Always take the time to talk with your pharmacist-even if you think you know everything.

Eddie Bennett
December 11, 2025 AT 20:20Been a pharmacist for 12 years. I used to skip the generic talk until I had a guy show up in the ER because he thought his blood pressure med was fake. Now I show the pill, say it plain, and ask them to repeat it back. Takes 90 seconds. Worth every second.
Mia Kingsley
December 12, 2025 AT 17:46Ugh another article about how pharmacists need to TALK more like we dont already have 12 patients screaming at us for their Xanax refill?? Like yeah sure lets add MORE steps to the chaos
Katherine Liu-Bevan
December 13, 2025 AT 01:49There’s a study from JAMA Internal Medicine in 2022 that tracked 18,000 patients on generics. Those who received structured counseling had a 41% lower discontinuation rate. The key isn’t just saying the words-it’s confirming understanding. Teach-back works because it’s not about what you said-it’s about what they heard.
Michaux Hyatt
December 14, 2025 AT 23:57I train new techs at my pharmacy. I tell them: 'Your job isn’t to count pills. It’s to make sure someone doesn’t die because they thought their heart med turned into a candy.' A printed chart with before/after pills? 50 cents. Saved three people last month alone.
Sylvia Frenzel
December 16, 2025 AT 00:54Why are we even talking about this? The FDA says it’s safe. If people are too dumb to trust the government, that’s not the pharmacist’s problem. Stop infantilizing adults.
Raj Rsvpraj
December 17, 2025 AT 08:12As an Indian pharmacist who trained in Mumbai, I can tell you: in the U.S., you overthink everything. In India, we hand over the pill, say 'Same medicine,' and move on. No forms. No checklists. No 'teach-back.' Patients trust us. Why? Because we’re not treating them like children.
Jack Appleby
December 17, 2025 AT 17:36Let’s be real-this whole ‘generic counseling’ movement is just corporate pharmacy’s attempt to monetize compliance. You think patients care about bioequivalence? They care about price. If the generic costs $4 instead of $40, they’ll take it-regardless of color, shape, or your PowerPoint presentation.
Frank Nouwens
December 18, 2025 AT 07:43While I appreciate the intent behind structured counseling protocols, one must acknowledge the systemic constraints under which community pharmacists operate. The average dispensing cycle, including verification, labeling, and insurance adjudication, exceeds 4.7 minutes. To impose an additional 90-second cognitive burden without structural support may be well-intentioned, yet logistically untenable.
Jim Irish
December 18, 2025 AT 10:30My grandma stopped her statin because the pill was green instead of white. She thought it was poison. I sat with her for 15 minutes, showed her the FDA page, and made her say it back: 'It’s the same medicine, just a different look.' She’s been on it for 3 years now. It’s not about the pill. It’s about the person.
Stephanie Maillet
December 18, 2025 AT 13:44There’s something deeply human here-this fear of the unfamiliar pill isn’t irrational. It’s a metaphor for how we all fear change when we don’t understand it. The pharmacist isn’t just explaining bioequivalence-they’re offering reassurance in a world that feels increasingly alien. That’s not protocol. That’s medicine as ritual.
Paul Dixon
December 19, 2025 AT 14:22My old man had a heart attack last year. He was terrified of the generic because it looked like a baby pill. My pharmacist didn’t just explain it-she drew it for him on a napkin. He still keeps that napkin in his wallet. That’s the kind of stuff that sticks.
Vivian Amadi
December 20, 2025 AT 00:39Anyone who thinks this is just about 'trust' is delusional. The real issue? Insurance companies forcing generics without any patient education. Pharmacists are the scapegoats for corporate greed. Stop blaming the people who are trying to fix a broken system.