Preparing for a Kidney Transplant: Evaluation, Waitlist, and Living Donors
 Dec, 1 2025
Dec, 1 2025
Waiting for a kidney transplant isn’t just about hoping for a call. It’s a long, detailed process that starts long before you’re placed on the waitlist. If you’re preparing for a transplant, you need to understand the steps: the medical and emotional evaluation, how the waitlist actually works, and what it means to have a living donor. This isn’t something you can rush. But if you know what to expect, you can move through it with more control and less stress.
How the Transplant Evaluation Really Works
The evaluation isn’t one appointment. It’s a series of tests, interviews, and paperwork that can take anywhere from 8 to 16 weeks. Most people start when their kidney function drops below an eGFR of 20. That’s when your nephrologist refers you to a transplant center. But getting started doesn’t mean you’re automatically approved. Every center follows strict national guidelines. You’ll need to prove you’re physically strong enough for surgery. That means blood tests for liver and kidney function, viral screenings for HIV and hepatitis, and heart checks like an echocardiogram and stress test. Your heart has to handle the strain of surgery and lifelong medication. If your ejection fraction is below 40%, or you can’t walk on a treadmill for five minutes, you’ll need more treatment first. Then there’s the immune system check. Your blood is tested for antibodies that might attack a new kidney. If your Panel Reactive Antibody (PRA) is high, you’re harder to match. That can mean a longer wait. Some centers now use a calculated PRA (cPRA) to prioritize patients who are hardest to match. You’ll also need cancer screenings. Men over 50 get a PSA test. Women get mammograms and Pap smears. If you’ve had cancer in the last five years, you’re likely not eligible-unless it’s a low-risk type that’s been in remission for years.The Psychosocial Side: Why It Matters More Than You Think
Most people think the medical tests are the hardest part. But for many, the psychosocial evaluation is the most stressful. A social worker and psychologist will sit down with you to ask hard questions: Who will help you after surgery? Can you get to appointments? Do you have money for medications? Can you stick to a daily pill schedule? It’s not about judging you. It’s about survival. One study found that 32% of people who fail evaluation do so because of psychosocial reasons-not medical ones. Missing appointments, not taking meds, or lacking support can lead to transplant failure. Centers want to make sure you won’t be alone after the surgery. You’ll need to show you can afford post-transplant care. Medications cost about $32,000 a year. Most centers require proof you have at least $3,500 in liquid savings to cover co-pays in the first year. Insurance helps-Medicare covers 80% of transplant costs, private insurers 70-90%-but gaps still exist. Insurance delays are the #1 reason evaluations stall. Some Medicaid patients wait 37 extra days just to get approval for tests.What Happens After You’re Cleared?
Once the transplant committee meets-usually once a week-they decide if you’re approved. You’ll get a decision within 72 hours. If you’re cleared, you’re added to the waitlist. But being on the list doesn’t mean you’ll get a kidney soon. As of January 2024, over 102,000 people in the U.S. were waiting for a kidney. The average wait is 3.6 years. That’s not a guess. It’s based on real data from the Organ Procurement and Transplantation Network. Your wait time depends on your blood type, how sensitized your immune system is, and how much time you’ve spent on dialysis. But there’s a faster path: a living donor. Nearly 40% of all kidney transplants in 2023 came from living donors. That’s because kidneys can be donated by someone who’s still alive. A healthy person can live perfectly fine with one kidney.Living Donors: How It Works and Who Can Be One
A living donor doesn’t have to be a family member. It can be a friend, coworker, or even a stranger who wants to help. The donor goes through their own evaluation-just as strict as yours. They need to be in excellent health, have normal kidney function, and be free of diabetes, high blood pressure, or cancer. The donor’s evaluation has been streamlined. Leading centers now use rapid crossmatch protocols that cut the process from 6-8 weeks down to 2-3 weeks. Blood type compatibility is key. Type O donors can give to anyone. Type AB recipients can receive from anyone. But even if you’re not a match, you’re not out of luck. The Kidney Paired Donation Program helps incompatible pairs. Let’s say your spouse wants to donate but isn’t a match. They can give to someone else, and in return, you get a kidney from another donor whose partner is compatible with you. In 2023, this program helped 1,872 people get transplants. Living donor transplants have better outcomes. The one-year graft survival rate is 96.3%, compared to 94.1% for deceased donor kidneys. Plus, you can schedule the surgery. No waiting. No dialysis during the wait.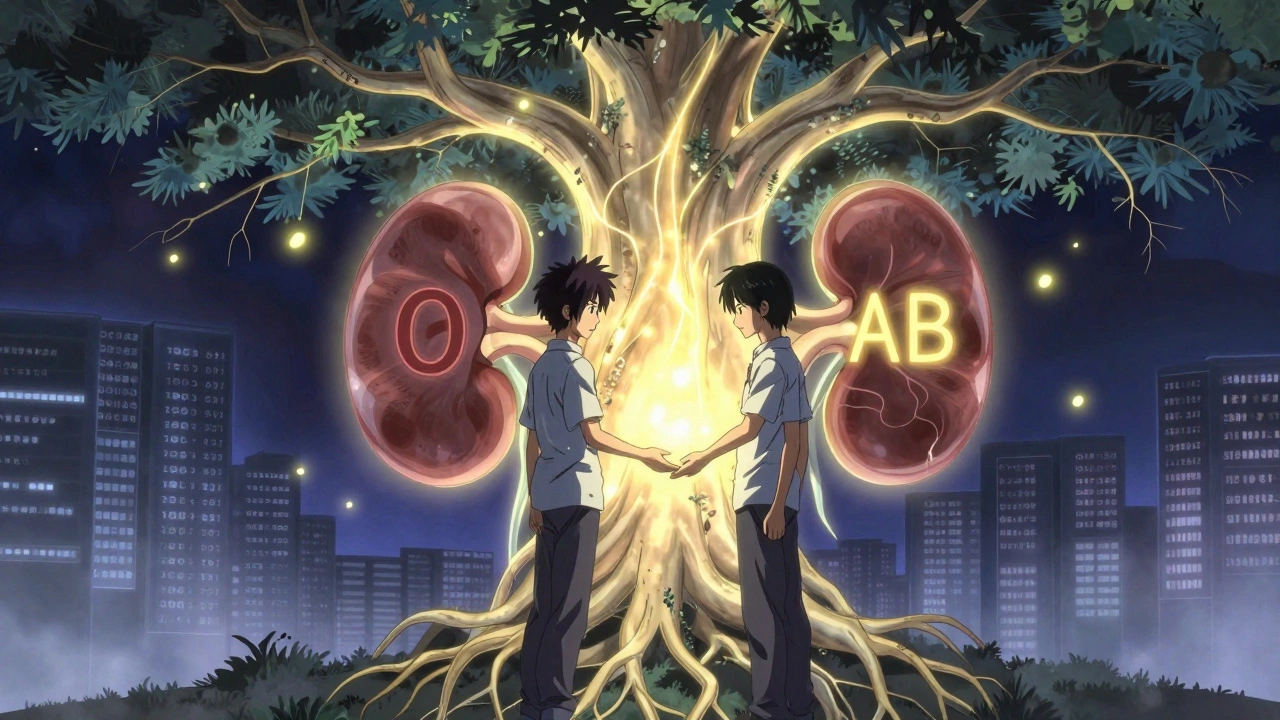
Why Some People Don’t Make It Through Evaluation
It’s not easy to qualify. The top five reasons people are turned down:- Active cancer (14.2%)
- Severe heart disease (11.8%)
- Uncontrolled infection (9.3%)
- Severe obesity (BMI over 40, 8.7%)
- History of not following medical advice (7.9%)
What You Can Do to Speed Things Up
You can’t control the waitlist. But you can control how fast you get through evaluation.- Get all your medical records ready-5 years’ worth, including dialysis logs if you’ve had them.
- Bring the same support person to every appointment. They’ll remember details you miss.
- Track every test result in your patient portal. Don’t wait for the center to call you.
- Call your insurance company early. Ask exactly what’s covered and what you’ll owe.
- Ask your transplant coordinator if you can do multiple tests in one day. High-volume centers can schedule 12 appointments in 6 weeks instead of 12.
- Start talking to people you know about being a donor. Don’t wait until you’re desperate.
What Happens After You’re Listed?
Once you’re on the list, your life becomes a balance of waiting and preparing. You’ll need to keep your phone charged and your contact info updated. The call can come at any time-day or night. You’ll need to be ready to get to the hospital within hours. You’ll also need to stay healthy. No smoking. No alcohol. Keep your weight stable. Avoid infections. If you get sick, call your transplant team immediately. A bad cold or UTI can delay your transplant. And you must keep taking your meds-even if you feel fine. Skipping dialysis or meds can get you removed from the list.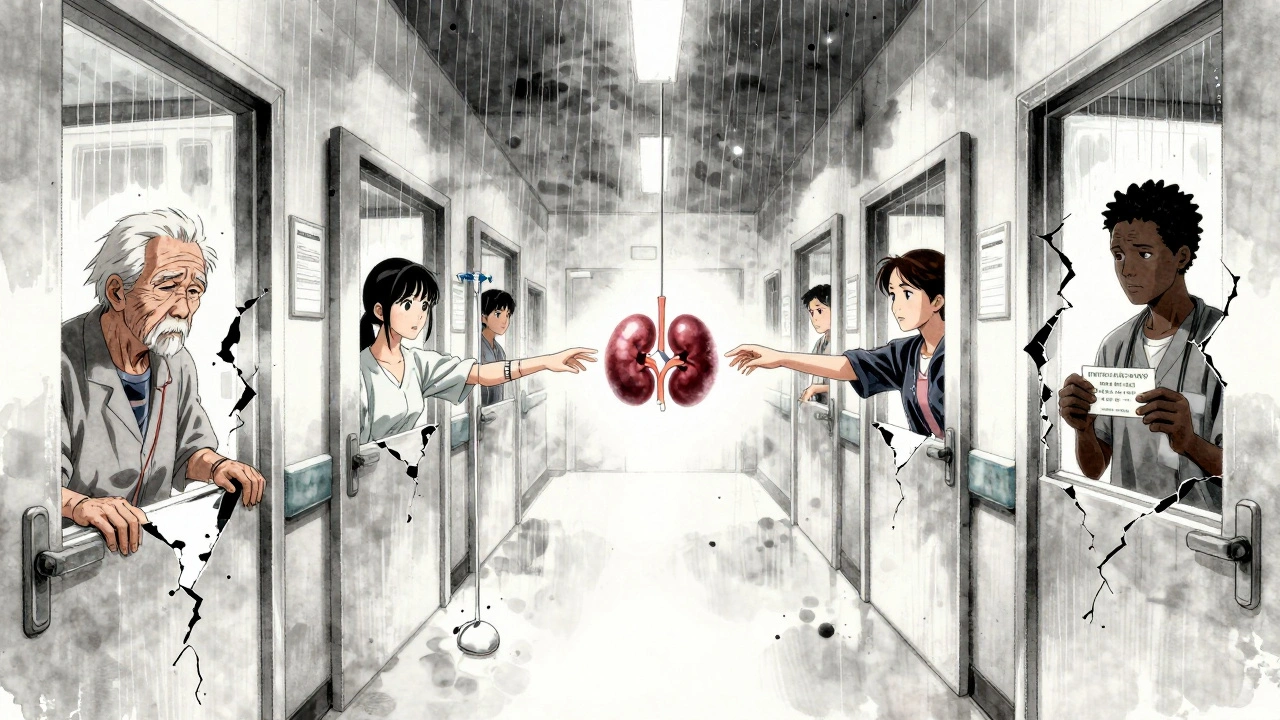
What’s Changing in 2025
The transplant system is slowly improving. The HOPE Act now allows HIV-positive donors to give to HIV-positive recipients-217 transplants happened this way in 2023, up from zero in 2013. New financial support rules under the End-Stage Renal Disease Transplant Act may reduce abandonment rates by 15-20% by 2026. But there’s still a shortage. Over 60% of transplant centers say they don’t have enough coordinators. That means longer wait times for evaluations. The goal by 2027 is to get 90% of people through evaluation within 120 days. Right now, only 68% make it through at low-volume centers.Final Thoughts: You’re Not Alone
This process is overwhelming. One patient on Reddit spent 17 appointments over 11 weeks just to finish evaluation. Another paid $8,200 out of pocket, even with insurance. But others found help. One person said their coordinator saved them six weeks by scheduling everything back-to-back. You don’t have to figure this out alone. Talk to your transplant team. Ask questions. Keep records. Find a support group. The goal isn’t just to survive the wait-it’s to be ready when the call comes.How long does the kidney transplant evaluation take?
The evaluation typically takes 8 to 16 weeks, depending on your health, insurance approval, and how quickly you complete tests. Living donor candidates often finish faster-around 8 to 12 weeks-because the donor’s evaluation can run in parallel. Deceased donor candidates usually take longer, averaging 12 to 16 weeks. High-volume transplant centers complete evaluations 23% faster than smaller ones.
Can I be on the transplant list if I’m on dialysis?
Yes, most people are placed on the waitlist while still on dialysis. In fact, being on dialysis is often a requirement for listing. The transplant team wants to see how you’re managing your health during dialysis, including your ability to follow treatment schedules and manage medications. Some centers prefer patients to be listed before starting dialysis if their kidney function is below 20 mL/min/1.73m², as early listing improves long-term survival.
What if I don’t have a living donor?
You can still be listed for a deceased donor kidney. About 60% of kidney transplants come from deceased donors. Your wait time will depend on your blood type, tissue match, and how sensitized your immune system is. People with common blood types (like O or A) and low antibody levels typically wait longer, while those with rare types or high antibody levels may get priority. The Kidney Paired Donation Program also helps if you later find a donor who isn’t a match for you.
How much does a kidney transplant cost, and is it covered?
The total cost of a kidney transplant can exceed $500,000, including surgery, hospital stay, and the first year of anti-rejection drugs. Medicare covers 80% of transplant-related costs under Part B, and Part D helps with prescription drugs. Private insurance usually covers 70-90% after you meet your deductible, which averages $4,550 per year. Medicaid coverage varies by state. Most transplant centers require proof you can afford $3,500 in out-of-pocket costs for medications in the first year. Financial assistance programs are available through organizations like the American Kidney Fund.
Can I be too old for a kidney transplant?
There’s no strict age limit for kidney transplants. Many patients over 70 receive transplants successfully. What matters more than age is your overall health. If you’re otherwise healthy-with good heart function, no active cancer, and the ability to manage medications-you’re a candidate. Transplant centers assess biological age, not calendar age. Studies show older patients who receive transplants live longer and have better quality of life than those who stay on dialysis.
What happens if I’m denied for a transplant?
If you’re denied, the transplant team will explain why. Common reasons include uncontrolled diabetes, active infection, severe heart disease, or psychosocial concerns like lack of support or non-adherence. Some denials are temporary. For example, if you’re overweight, you may be asked to lose weight and reapply. If you have an infection, you may be cleared after treatment. You can request a second opinion from another transplant center. Many centers have different criteria, especially for borderline cases.

Jay Everett
December 3, 2025 AT 07:18Man, this post hit different. I spent 14 months getting cleared and honestly? The psychosocial eval was worse than the stress tests. They asked me if I’d still take my meds if I got depressed after surgery. Like… yeah? I’m not an idiot. But they needed proof I wasn’t just saying what they wanted to hear. One social worker cried when I told her I’d been sleeping in my car between shifts to save money for meds. She didn’t say anything, just nodded. That meant more than any approval letter.
And yeah, living donors? My cousin gave me a kidney. We weren’t even close before. Now? We’re weirdly inseparable. She says she didn’t do it for gratitude. She did it because she couldn’t stand seeing me limp around like a ghost. I just hope someone else finds their person like that.
Also, the PRA thing? Mine was 98%. They told me I’d wait 7 years. Got the kidney in 18 months. Turns out, being a nightmare to match works in your favor. Weird system.
PS: If you’re on Medicaid, call your coordinator every damn day. They’re drowning. I sent 47 emails. Got my tests scheduled in 3 weeks. No one else did. You gotta be the squeaky wheel.
Elizabeth Grace
December 3, 2025 AT 17:49I’m 62 and got approved last year. They said I was ‘too old’ at 58. Then I lost 40 lbs, quit smoking, and started walking 5 miles a day. Now I’m on the list. Age is just a number. Your body’s the real judge. Don’t let them tell you you’re too old to fight.
Also… I cry every time I see my donor’s name on my meds. She’s 28. I call her my angel. Don’t be afraid to ask for help. We’re all just trying to stay alive.
Alicia Marks
December 5, 2025 AT 05:39You got this. One step at a time. You’re not alone.
Laura Baur
December 5, 2025 AT 12:39Let’s be honest: the system is rigged. You need money, connections, and perfect compliance to survive this. The fact that Medicaid patients wait 37 extra days just to get basic tests approved is a moral failure. And don’t get me started on racial disparities. They say ‘standardized pathways’ fixed it? That’s PR spin. The data still shows Black patients wait longer, even when controlling for everything. This isn’t healthcare-it’s a lottery with stacked decks.
And don’t tell me ‘just be more proactive.’ When you’re working two jobs and your kid has asthma, you don’t have time to chase insurance reps. The system should adapt to real human lives, not the other way around.
dave nevogt
December 5, 2025 AT 23:46There’s a philosophical paradox here: the more you fight to survive, the more the system demands you perform your survival. You must be disciplined, organized, emotionally stable, financially solvent, and socially connected-all while your body is failing. The transplant process doesn’t just test your kidneys. It tests your soul’s capacity to be perfect under pressure.
And yet, the people who fail aren’t lazy or weak. They’re often the ones who’ve already survived homelessness, abuse, or systemic neglect. The psychosocial eval isn’t about ‘readiness.’ It’s about who the system deems worthy of a second chance. That’s not medicine. That’s judgment dressed in white coats.
I watched a man get denied because he missed one appointment after his mother died. He was grief-stricken. The team said ‘non-adherence.’ He wasn’t non-adherent. He was human.
Maybe the real transplant isn’t the kidney. Maybe it’s the society that learns to stop punishing people for being broken.
Steve World Shopping
December 7, 2025 AT 18:44Baseline: PRA > 80% = Class 4 sensitization = high immunologic risk. cPRA > 95% = virtual crossmatch required. Standard of care mandates pre-transplant HLA antibody screening via Luminex. Non-compliance with immunosuppression protocols = 5x higher risk of AMR. You need to understand that this isn’t a DIY process-it’s a complex immunological cascade requiring multidisciplinary coordination. If you’re not tracking your eGFR trends and medication adherence via EHR, you’re gambling with graft survival.
Also, living donor logistics: ABO compatibility, crossmatch negativity, and donor renal function must meet KDIGO guidelines. Don’t assume ‘anyone can donate.’ Only 3% of potential donors pass screening. It’s not altruism-it’s a rigorous clinical pathway.
Steve Enck
December 7, 2025 AT 23:20Let’s deconstruct the narrative. The article frames this as a journey of resilience. But resilience is a capitalist myth. The fact that you must prove your worthiness to receive a life-saving organ is not a feature-it’s a pathology. The system incentivizes compliance over compassion. It rewards those with social capital, financial literacy, and emotional performative stability.
Why is the burden of proof placed on the sick? Why does the state not guarantee access to care as a right? Why do we celebrate donors as saints while ignoring that the entire system is built on scarcity, not equity?
This isn’t medicine. It’s moral theater. And we’re all just actors in a play where the script was written by actuaries.
Lynn Steiner
December 9, 2025 AT 09:57I’m crying. I’m 32 and on dialysis. I’ve been waiting 2 years. I’ve had 14 appointments. My insurance denied my cardiac stress test TWICE. I had to pawn my grandma’s necklace to pay for it. I don’t have a donor. I don’t know if I’ll ever get one. I just want to hold my nephew without being too tired to lift him.
Why is this so hard? Why does it feel like the world wants me to just… give up?
💔
Roger Leiton
December 9, 2025 AT 23:00Just wanted to say-this thread is everything. I’m 19 and got diagnosed with FSGS last year. I didn’t know what any of this meant. I thought ‘transplant’ meant ‘magic fix.’ Turns out it’s a whole other life.
My mom is trying to be my donor. We’re doing the testing next month. I’m scared. But reading this? It made me feel less alone.
Also-can someone explain the paired donation thing again? I think I get it but I wanna make sure I’m not missing something 😅
मनोज कुमार
December 11, 2025 AT 16:32Joel Deang
December 13, 2025 AT 00:09yo so i just found out my bro wants to be my donor and i’m literally bawling rn like… how do u even thank someone for giving you a part of themselves??
also i’m from texas and my insurance said ‘no’ to the pre-transplant ct scan so i had to go to a free clinic and they did it for 80 bucks. i’m so grateful. u guys are my heroes. 🙏❤️
Jack Dao
December 13, 2025 AT 19:11Let me be clear: this entire system is a failure of moral imagination. You’re not ‘waiting’ for a kidney. You’re begging for charity from a broken system that treats human life as a commodity. The fact that you must prove you’re ‘deserving’ of a transplant is the most dehumanizing aspect of modern healthcare.
And don’t tell me ‘living donors are heroes.’ They’re not heroes. They’re people who stepped into a system that failed everyone else. The real heroes are the ones who never got the chance because they were poor, Black, or didn’t have a network.
Stop glorifying survival. Start demanding justice.