Psoriasis and Beta-Blockers: What You Need to Know About Skin Flare Risk
 Oct, 31 2025
Oct, 31 2025
Beta-Blocker Psoriasis Risk Calculator
If you have psoriasis and are taking a beta-blocker for high blood pressure or heart issues, your skin flare-ups might not be random. They could be linked to the medication itself. While beta-blockers save lives by lowering heart rate and blood pressure, they’re also one of the most common drugs known to make psoriasis worse - sometimes even triggering it in people who never had it before.
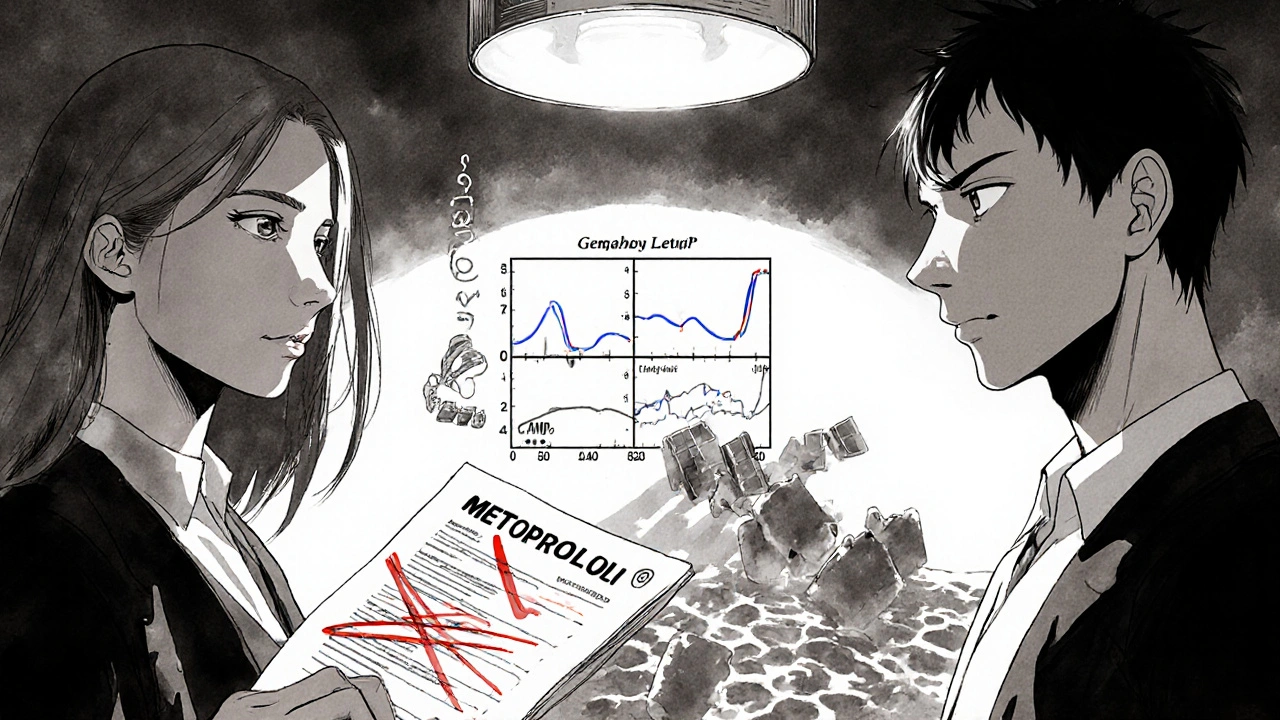
How Beta-Blockers Can Trigger Psoriasis Flares
Beta-blockers like metoprolol, propranolol, and atenolol work by blocking adrenaline from binding to beta receptors in your heart and blood vessels. That’s good for your cardiovascular system. But those same receptors are also found in your skin. When beta-blockers interfere with them, they disrupt the normal balance of skin cell growth and inflammation.
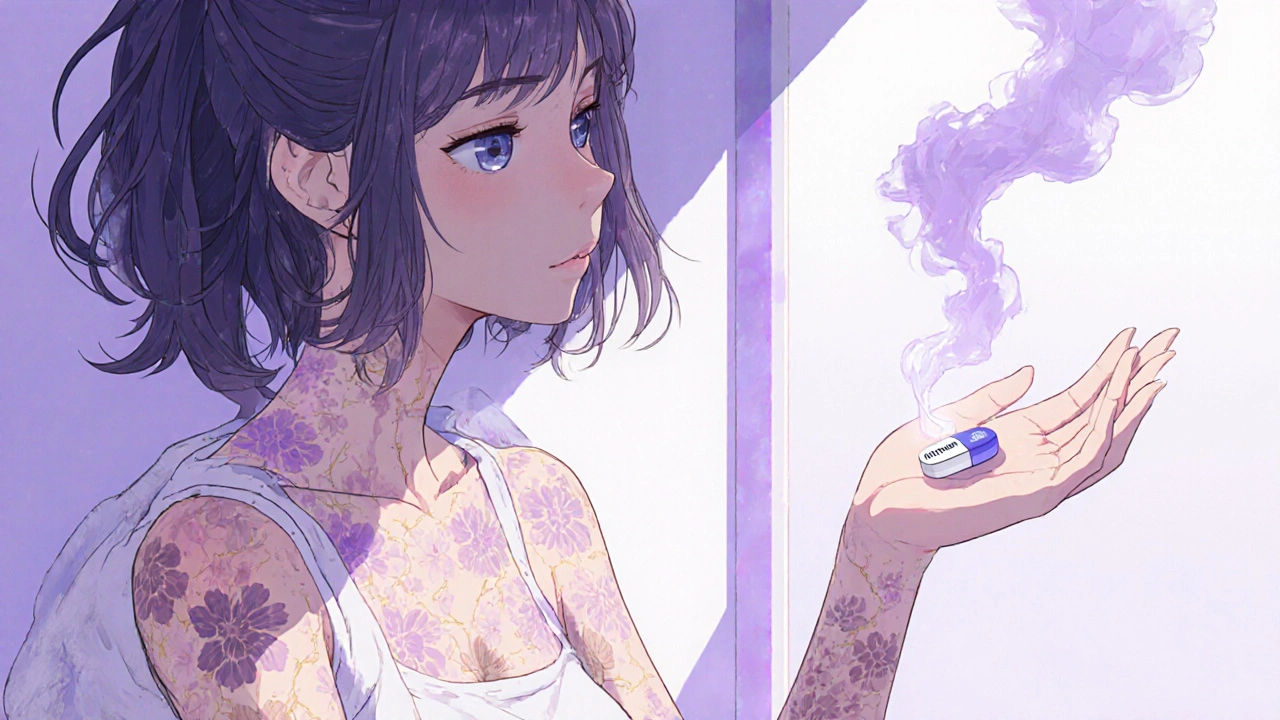
Research shows this happens because beta-blockers lower levels of cyclic AMP (cAMP), a molecule that helps regulate how skin cells behave. Lower cAMP means skin cells multiply too fast and immune cells in the skin get overactive - two hallmarks of psoriasis. This isn’t just theory. Case studies show people developing pustular psoriasis or even full-body redness (erythroderma) after starting beta-blockers, especially topical ones like timolol eye drops used for glaucoma.
It’s not always immediate. Flares can show up anywhere from one to 18 months after you start the medication. That delay is why many patients never connect their worsening skin to their heart pill. One man on Reddit shared that after six months on metoprolol, his psoriasis went from covering 5% of his body to 30%. He thought it was stress - until his dermatologist asked about his meds.
Which Beta-Blockers Are Most Likely to Cause Problems?
Not all beta-blockers are created equal when it comes to skin risk. The ones most often linked to psoriasis flares are:
- Propranolol (Inderal)
- Metoprolol (Lopressor, Toprol-XL)
- Bisoprolol
- Atenolol (Tenormin)
- Pindolol (Visken)
- Timolol (eye drops for glaucoma)
Metoprolol is the most commonly prescribed beta-blocker in the U.S., with over 63 million prescriptions filled in 2023 alone. That means millions of people with psoriasis could be taking it without knowing the risk. DermNet NZ reports that about 20% of people with existing psoriasis see their condition worsen after starting one of these drugs. And in some cases, people without prior psoriasis develop it for the first time.
Here’s the twist: some beta-blockers seem safer. Nebivolol and carvedilol, for example, have fewer reports of skin side effects. But if one beta-blocker triggers your psoriasis, chances are another one will too. Banner Health’s 2023 guidance says doctors usually won’t try switching to a different beta-blocker - they’ll look for a whole different class of medication.
What Does the Evidence Really Say?
There’s conflicting science. A 2010 study in the Journal of the American Academy of Dermatology found beta-blockers were a major trigger for severe psoriasis flare-ups. But another paper from the same year argued that cumulative exposure to beta-blockers wasn’t a strong risk factor. Why the contradiction?
It comes down to individual biology. Genetics play a big role. People with the HLA-C*06:02 gene variant - which is linked to early-onset plaque psoriasis - may be more likely to react badly to beta-blockers. A 2024 study at Johns Hopkins and Mayo Clinic is testing whether this gene can predict who’s at highest risk. Early results suggest it might.
Also, not everyone reacts the same. Some patients take beta-blockers for years with no skin issues. Others flare up after just a few months. That variability makes it hard to spot the connection without a doctor’s help.
What Should You Do If You Suspect Your Med Is Causing Flares?
If you’ve noticed your psoriasis getting worse since starting a beta-blocker, don’t stop the medication on your own. Stopping suddenly can cause dangerous spikes in blood pressure or heart rate.
Instead, talk to both your dermatologist and cardiologist together. Bring a list of your medications and note when your skin changes started. Your dermatologist may ask: “When did you start this pill?” - a question most patients don’t expect.
If beta-blockers are the culprit, switching is usually the best option. Alternatives with lower psoriasis risk include:
- Calcium channel blockers like amlodipine
- ARBs like losartan or valsartan
Be careful: ACE inhibitors (like lisinopril) can also trigger psoriasis in some people, so they’re not always a safe swap. Your doctor will pick the best alternative based on your heart health, kidney function, and other conditions.
How Is Beta-Blocker-Induced Psoriasis Treated?
Once the trigger is removed, skin often improves - but not always right away. Treatment still follows standard psoriasis protocols:
- Topical steroids to reduce inflammation
- Vitamin D analogues like calcipotriene to slow skin cell growth
- Phototherapy (UVB light) for moderate to severe cases
- Systemic drugs like methotrexate or biologics if the flare is widespread
Many patients find that once the beta-blocker is out of their system, their skin responds better to these treatments. One woman on MyPsoriasisTeam wrote: “I switched from metoprolol to amlodipine. Within three months, my plaques were half the size. I finally slept through the night without itching.”
Why This Matters for Millions of People
Psoriasis affects over 8 million Americans. Beta-blockers are prescribed over 150 million times a year in the U.S. That means tens of thousands of people with psoriasis are on these drugs - and many don’t know the connection.
MedicalNewsToday’s 2023 survey found that 37% of psoriasis patients on beta-blockers reported worsening skin, compared to just 12% on other blood pressure meds. That’s a big difference. Yet most guidelines still list beta-blockers as a standard option for hypertension, even in patients with psoriasis.
The European Academy of Dermatology and Venereology now recommends that dermatologists always ask patients with new or worsening psoriasis: “Are you on any heart medications?” This simple question could prevent months of unnecessary suffering.
What’s Next? Better Options on the Horizon
Drug companies are working on new beta-blockers that target only the heart’s beta-1 receptors and leave skin receptors alone. Early animal studies show promise. If successful, these could be available in the next 5-7 years.
In the meantime, awareness is key. If you have psoriasis and are on a beta-blocker, ask your doctor: “Could this be making my skin worse?” If you’re on a beta-blocker and just developed psoriasis, ask: “Could this be drug-induced?”
There’s no shame in needing heart medication. But there’s power in knowing how your drugs affect your whole body - not just your heart.
Can beta-blockers cause psoriasis in people who never had it before?
Yes. While beta-blockers are more likely to worsen existing psoriasis, they can also trigger the condition in people who didn’t have it. Case reports show new-onset psoriasis appearing after starting metoprolol, propranolol, or even topical timolol eye drops. The risk is lower than for flare-ups in existing patients, but it’s real and documented in medical literature.
How long after starting a beta-blocker does psoriasis usually flare up?
There’s no set timeline. Flares can happen as early as one month after starting the medication, or as late as 18 months. This delayed reaction is why many people don’t realize their skin issue is drug-related. If your psoriasis suddenly gets worse months after starting a new heart pill, it’s worth discussing with your doctor.
If one beta-blocker causes a flare, will others do the same?
Most likely, yes. Beta-blockers work in similar ways, and if your skin reacts to one, it’s probably reacting to the class effect - not just a single drug. Doctors typically avoid switching to another beta-blocker and instead move to a different class of blood pressure medication, like a calcium channel blocker or ARB.
Are there any beta-blockers that are safer for psoriasis patients?
Some beta-blockers appear to have lower skin risk. Nebivolol and carvedilol have fewer reported cases of psoriasis flares compared to metoprolol or propranolol. However, there’s no guarantee they’re safe for everyone. The safest approach is to avoid the entire class if you’ve had a reaction - and choose an alternative medication instead.
Can I stop my beta-blocker if I think it’s making my psoriasis worse?
No. Stopping beta-blockers suddenly can cause dangerous spikes in blood pressure, heart rate, or even heart attack. Always talk to your doctor first. They can help you switch safely - often by gradually reducing the dose while starting a new medication. Never make this change on your own.

Adarsha Foundation
November 1, 2025 AT 22:05Interesting read. I’ve been on metoprolol for years and my psoriasis has been stable, but I never connected the dots. Maybe I’m one of the lucky ones-or maybe my body just handles it better. Either way, good to know this exists.
Alex Sherman
November 3, 2025 AT 10:39Of course the medical establishment ignores this. They’re too busy pushing pharmaceuticals to care about side effects that aren’t immediately lethal. You think they want you to know your blood pressure med is turning your skin into a battlefield? Please.
Oliver Myers
November 4, 2025 AT 07:13This is such an important topic-and thank you for laying it out so clearly. I’ve seen patients come in with severe flares, and when we ask about meds, it’s often a beta-blocker. It’s not always obvious, but once you connect the dots, things improve so much. Seriously, if you’re on one and your skin’s acting up, talk to your docs. Don’t guess. Don’t stop cold. Just ask.
John Concepcion
November 4, 2025 AT 14:10Wow, someone actually wrote a whole article about this? I thought everyone knew beta-blockers wreck your skin. Like, duh. My cousin got pustular psoriasis after starting atenolol-she thought it was ‘stress’ for six months. Then her dermatologist said, ‘Did you take your heart pill?’ She cried. So did I. Thanks for the reminder that doctors are clueless.
Caitlin Stewart
November 4, 2025 AT 15:15I’m a nurse in a dermatology clinic, and this comes up more than you’d think. Patients are always shocked when we ask, ‘When did you start this med?’-because they never think to connect the two. I’ve had people say, ‘I thought my skin just got worse with age.’ No, honey. It’s the metoprolol. We’ve seen it so many times. Please, if you’re on one and your plaques are flaring, don’t suffer silently. Bring this up. It’s not a weird question.
Emmalee Amthor
November 4, 2025 AT 21:56People always think medicine is perfect, but the truth? It’s just a bunch of trial and error with side effects nobody talks about. I got psoriasis after starting metoprolol. Took me a year to figure it out. I switched to amlodipine and my skin cleared up 80%. Now I’m not just surviving-I’m living. Don’t let fear of stopping meds keep you in pain. Talk to your doctors. Be your own advocate. You’re worth more than a pill that makes you itch.
Leslie Schnack
November 6, 2025 AT 20:13Has anyone looked into whether the route of administration matters? Like, topical timolol eye drops causing psoriasis? That’s wild. I never thought eye drops could affect your skin like that. Makes me wonder what other ‘local’ meds are doing systemic damage we don’t know about.
Saumyata Tiwari
November 8, 2025 AT 06:15Why are Americans so obsessed with blaming drugs for everything? In India, we’ve been using beta-blockers for decades and psoriasis is still rare. It’s not the medicine-it’s your diet, your stress, your laziness. Stop looking for external villains and fix your lifestyle. Maybe then you won’t need so many pills.
Anthony Tong
November 9, 2025 AT 13:33Big Pharma is hiding this. They know beta-blockers trigger psoriasis. They know it’s common. But they don’t want you to know, because then you’d stop taking them. And if you stop, they lose billions. This is why the FDA never issues warnings. This is why your doctor doesn’t ask. This is why they’re all on the payroll. Wake up.
Roy Scorer
November 9, 2025 AT 17:58It’s not about the drug-it’s about the soul. Beta-blockers suppress the body’s natural rhythm, and psoriasis is the body screaming back. The skin is the mirror of the spirit. When you silence the heart’s song with chemicals, the soul retaliates through the epidermis. This isn’t medicine-it’s spiritual dissonance dressed in white coats.
Marcia Facundo
November 10, 2025 AT 13:19I just want to say I’ve been on carvedilol for three years and my psoriasis is fine. So maybe it’s not everyone? Or maybe I’m just lucky? Either way, I’m glad someone’s talking about this. I didn’t even know this was a thing.
Ajay Kumar
November 12, 2025 AT 01:45Look, I get it, beta-blockers might be bad for psoriasis, but let’s not ignore the fact that in 2023, over 63 million prescriptions for metoprolol were filled in the U.S. alone. That’s millions of people who are alive because of this drug. If you have a mild flare-up, maybe you should consider whether your life or your skin is more important? I’m not saying ignore it, but don’t throw the baby out with the bathwater. Also, I’ve been on propranolol for 12 years and my skin is fine, so maybe it’s not the drug-it’s your genetics, your gut, your aura, your aura is bad, I can feel it.
Hazel Wolstenholme
November 12, 2025 AT 05:35How quaint. We’re all so eager to reduce complex immunological phenomena to a single pharmacological villain. The truth? Psoriasis is a symphony of dysregulation-genetic predisposition, microbiome collapse, environmental triggers, psychological stress, and yes, perhaps beta-blockers as one dissonant note in a cacophonous orchestra. To isolate one agent as ‘the cause’ is not science-it’s reductionist fantasy. And yet, we cling to it, because simplicity soothes the anxious mind. But let’s not mistake comfort for truth.
Mike Laska
November 13, 2025 AT 01:35My mom took metoprolol for 8 years. Her skin went from ‘mild patches’ to full-body redness. She cried every night. She didn’t tell anyone because she was scared to stop her heart med. When she finally switched to losartan, it took 4 months, but the relief? Like waking up from a nightmare. I’m so glad this is out there. Please, if you’re reading this and you’re on a beta-blocker and your skin’s on fire-don’t wait. Talk to your doctor. I’m not a doctor, but I’ve seen what silence does.