Renal Nutrition: Protein Targets for CKD Stages Explained
 Dec, 16 2025
Dec, 16 2025
When your kidneys aren't working well, what you eat matters more than you might think. Especially protein. Too much can overload your kidneys. Too little can leave you weak and malnourished. Finding the right balance isn’t about cutting protein entirely-it’s about getting the right amount for your stage of kidney disease. This isn’t guesswork. It’s science-backed, personalized nutrition that can slow damage, delay dialysis, and help you feel better day to day.
What Protein Does to Your Kidneys
Your kidneys filter waste from your blood. When you eat protein, your body breaks it down into nitrogen-based waste like urea. Healthy kidneys handle this easily. But when kidney function drops, that waste builds up. That’s why protein intake is carefully managed in chronic kidney disease (CKD). The goal isn’t to starve your body-it’s to reduce the strain so your kidneys don’t work overtime. Studies show that keeping protein in the right range can slow the decline of kidney function by up to 32%, according to the 2022 Cochrane Review. For many, that means pushing back dialysis by six to twelve months.
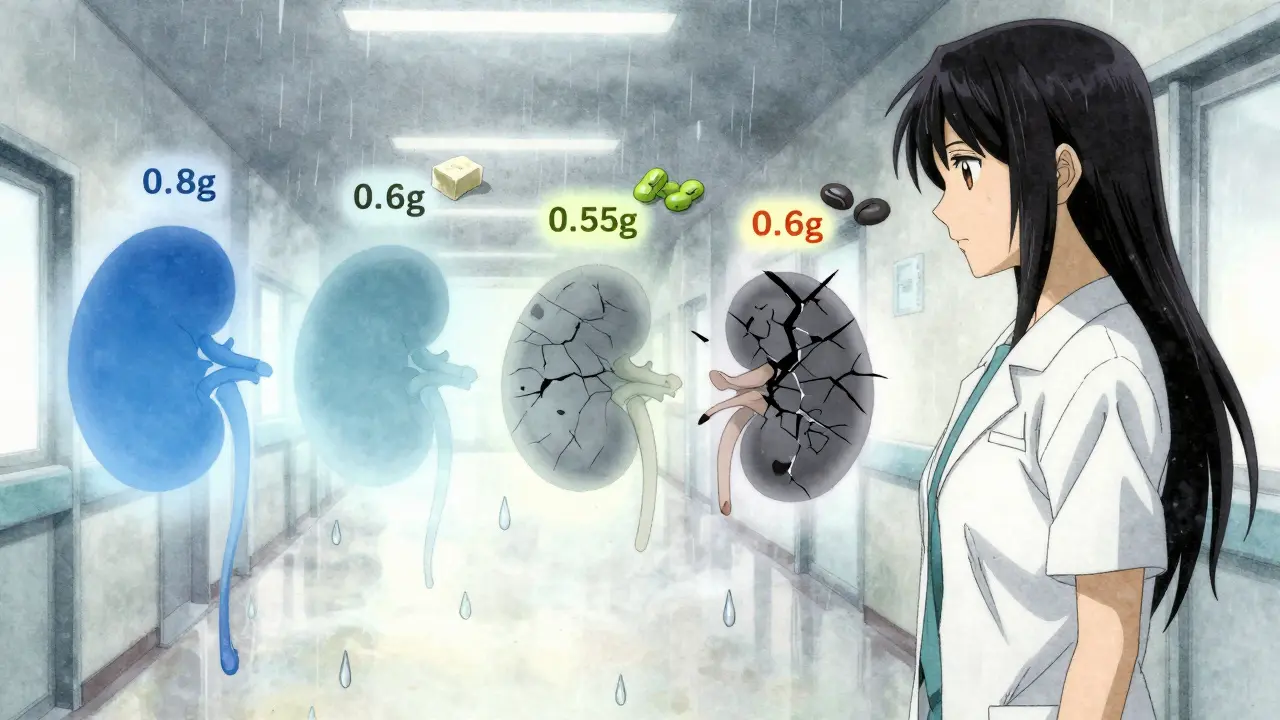
Protein Targets by CKD Stage
Not all CKD is the same. Your protein needs change as your kidneys decline. Here’s what the latest guidelines say:
- CKD Stage 1-2 (GFR ≥60): Your kidneys are still working fairly well. Most experts recommend no more than 0.8 grams of protein per kilogram of ideal body weight. For someone weighing 150 lbs (68 kg), that’s about 54 grams per day. But new research from JAMA Network Open in 2024 suggests that for older adults, slightly higher intake-up to 1.0 g/kg-may actually lower death risk without speeding kidney damage.
- CKD Stage 3 (GFR 30-59): This is where careful planning becomes critical. The standard target is 0.55-0.60 g/kg per day. That’s roughly 40-54 grams daily for a 150 lb person. But if you’re also diabetic, the American Diabetes Association recommends 0.8-0.9 g/kg to avoid muscle loss while still protecting your kidneys.
- CKD Stage 4 (GFR 15-29): Protein drops further to 0.6 g/kg. Half of that protein should come from high-quality sources-eggs, milk, chicken, fish, lean beef, or soy. These contain all the essential amino acids your body can’t make on its own.
- CKD Stage 5 (GFR <15, not on dialysis): Protein stays around 0.6 g/kg, but many patients here are at high risk of protein-energy wasting. About 30-50% of stage 3-5 patients develop this condition, according to NHANES data. That’s why protein restriction here is never done alone-it’s paired with calorie support and often medical foods like keto acid analogues.
Plant vs. Animal Protein: The Real Difference
Not all protein is created equal when it comes to kidney health. Animal proteins-like steak, chicken, and cheese-produce more urea and phosphate per gram than plant proteins. They also generate more advanced glycation end products (AGEs), which cause inflammation and oxidative stress in people with kidney disease.
Plant proteins-beans, lentils, tofu, nuts, and whole grains-create 20-30% less waste. A 2021 meta-analysis in the Clinical Journal of the American Society of Nephrology found that replacing just 30% of animal protein with plant protein lowered the risk of CKD progression by 14% and reduced death risk by 11%. That’s huge.
But here’s the catch: plant proteins often lack one or more essential amino acids. Lysine and methionine, for example, are harder to get from plants alone. That’s why combining them matters-rice and beans, hummus and whole wheat pita, tofu with quinoa. You need variety to cover all your bases.
Also, plant foods tend to be high in potassium. For someone in stage 4 or 5 CKD, that’s a problem. Too much potassium can cause dangerous heart rhythms. So while plant proteins are kidney-friendly, they require smart choices. Avoid high-potassium options like spinach, potatoes, and bananas. Stick to lower-potassium plants like cabbage, cauliflower, apples, and blueberries.
The Human Side of Protein Restriction
It’s one thing to know the numbers. It’s another to live them.
On patient forums like the American Kidney Fund’s, 68% of respondents said they struggled to stick to low-protein diets. The biggest complaints? Constant hunger (74%), muscle weakness (62%), and feeling isolated during meals (58%). One Reddit user wrote: “Cutting my protein from 100g to 45g daily made me feel like I was falling apart.”
But there’s hope. Patients who work with a renal dietitian are 82% more likely to stick with their plan, according to DaVita’s 2023 survey. Why? Because dietitians don’t just give numbers-they give meals. They help you build plates that fit your life: a breakfast of egg whites with toast, a lunch of rice and tofu stir-fry, a dinner of grilled chicken breast with cauliflower mash.
Tools like the National Kidney Foundation’s “Protein Target Calculator” app, downloaded over 47,000 times since 2023, make tracking easier. Apps like MyFitnessPal with renal databases help too. And meal prepping-using kidney-friendly recipes from sites like Kidney Kitchen, visited 1.2 million times a month-cuts daily stress.
What to Avoid and What to Try
Here’s what doesn’t work:
- Skipping meals to cut protein-this leads to muscle loss.
- Relying on protein shakes or bars unless they’re specially formulated for kidney disease. Most are loaded with phosphorus and potassium.
- Going too low without supervision. A 2023 study showed that patients who dropped below 0.5 g/kg without medical guidance had higher rates of malnutrition and hospitalization.
Here’s what does:
- Using keto acid analogues (like Ketosteril) if prescribed. These provide amino acid building blocks without the nitrogen waste. Used in 15% of stage 4-5 patients in Europe.
- Choosing lean proteins: skinless chicken, white fish, egg whites, tofu.
- Adding calorie-dense, kidney-safe carbs: white rice, pasta, bread, and oils to prevent your body from breaking down muscle for energy.
- Monitoring your weight weekly. A sudden drop of more than 2 pounds in a week could signal muscle loss.

Getting the Right Support
Most nephrologists know protein matters. But only 35% of them routinely refer patients to renal dietitians, even though guidelines say they should. That’s a gap in care.
Medicare now covers up to 3 hours of initial nutrition counseling and 2 hours of follow-up each year for CKD patients. That’s a big step. But you have to ask for it. Don’t wait until you’re weak or losing weight. Get a referral early.
Structured programs-where you meet a dietitian every 4-6 weeks, track your food, and adjust your plan-boost adherence by over 3 times. Patients in these programs stick to their diet 78% of the time. Those without support? Only 24%.
The Future of Kidney Nutrition
Research is moving beyond one-size-fits-all protein targets. The NIH-funded PRECISE-CKD trial is testing whether protein needs should be based on your body’s actual urea production-not just your weight. Some people naturally make more waste than others, even at the same weight.
Companies are also developing plant-based protein concentrates with reduced potassium. Imagine a soy protein powder that’s safe for stage 4 CKD. That’s not science fiction anymore.
And AI is stepping in. The American Society of Nephrology launched personalized protein algorithms in 2024. They use your lab values, genetics, and eating habits to predict how your body responds to different protein levels. This isn’t just about numbers anymore-it’s about precision.
One thing’s clear: protein management isn’t going away. In fact, 92% of nephrologists surveyed in early 2024 believe it will remain a core part of CKD care through 2030. But the focus is shifting-from how much you eat, to what kind you eat, and how your body uses it.
How much protein should I eat if I have stage 3 CKD?
For stage 3 CKD, aim for 0.55 to 0.60 grams of protein per kilogram of your ideal body weight. If you weigh 150 lbs (68 kg), that’s about 40-54 grams daily. Half of that should come from high-quality sources like eggs, fish, chicken, or soy. Always check with your dietitian-your needs may vary if you’re diabetic, older, or losing weight.
Can I eat beans and lentils with kidney disease?
Yes, but with caution. Beans and lentils are plant proteins that are easier on the kidneys than meat, but they’re also high in potassium and phosphorus. If you’re in stage 4 or 5, limit portions to 1/2 cup cooked per day, and soak them overnight to reduce minerals. Pair them with low-potassium foods like white rice or pasta. Always monitor your blood levels.
Why do I feel weak on a low-protein diet?
Feeling weak often means your body is breaking down muscle for energy because you’re not getting enough calories. Low-protein diets must be paired with enough carbs and healthy fats-like white rice, pasta, bread, olive oil, and butter-to prevent muscle loss. Talk to your dietitian about adding calorie-dense, kidney-safe foods. You shouldn’t feel exhausted.
Should I take protein supplements?
Most store-bought protein powders and bars are unsafe for CKD-they’re loaded with phosphorus, potassium, and additives. Only use supplements prescribed by your doctor or dietitian, like keto acid analogues (Ketosteril). These provide amino acids without the waste your kidneys can’t handle. Never self-prescribe protein shakes.
Is a vegan diet safe for kidney disease?
A well-planned vegan diet can be kidney-friendly and may slow progression, but it’s not automatic. You must carefully combine plant proteins to get all essential amino acids, limit high-potassium foods, and ensure enough calories. Many patients need supplements or fortified foods. Work with a renal dietitian to avoid malnutrition. It’s possible-but it’s not easy without expert help.
How often should I see a renal dietitian?
Start with an initial 60-90 minute session, then follow up every 4-6 weeks. Your needs change as your kidney function changes. If you’re losing weight, feeling weak, or your lab values shift, schedule an appointment sooner. Medicare covers 3 hours of initial counseling and 2 hours of follow-up yearly-use it.
Next Steps
If you’re managing CKD, don’t wait until you’re struggling to act. Get your protein target from your nephrologist or dietitian. Download the NKF Protein Calculator app. Start tracking your meals with a renal-friendly database. Ask about Medicare-covered nutrition counseling. And remember: this isn’t about perfection. It’s about progress. Small, consistent choices-like choosing egg whites over sausage, or white rice over brown-add up. Your kidneys will thank you.

Jane Wei
December 17, 2025 AT 11:26so i’ve been on a low-protein diet for my stage 3 ckd and honestly? i felt like a zombie for the first month. then i switched to mostly plant-based proteins and added eggs - boom, energy came back. no more brain fog. also, my nephrologist said i’m holding steady. weird how it works, right?
Jody Patrick
December 18, 2025 AT 21:50protein is poison for kidneys. cut it. period.
Radhika M
December 19, 2025 AT 17:08if you’re stage 3, aim for 0.6g per kg. chicken, eggs, tofu. avoid processed meats. drink water. simple. your kidneys will thank you.
Philippa Skiadopoulou
December 19, 2025 AT 21:30the data supporting protein restriction in early CKD remains inconclusive. while some studies suggest benefit, others show no significant difference in eGFR decline. individualization is key.
Pawan Chaudhary
December 20, 2025 AT 21:45you got this! even small changes make a big difference. i started with swapping beef for lentils and now i feel lighter than ever. keep going 💪
CAROL MUTISO
December 22, 2025 AT 17:16so let me get this straight - we’re told to eat less protein to save our kidneys, but if we eat too little we turn into walking skeletons? thanks, medicine. you’re really good at giving us impossible choices. also, who decided that 0.8g/kg is the magic number? some guy in a lab who hasn’t eaten a real meal since 1998?
my grandma ate bacon every day at 80 and still walked 3 miles. maybe we’re overcomplicating this.
Martin Spedding
December 24, 2025 AT 08:19protein = bad. eat veg. no meat. done.
also ur spelling is wrong in the post. its 'gfr' not 'GFR'. lol
amanda s
December 25, 2025 AT 08:10why are we even talking about this? americans are too lazy to cook real food. if you can’t follow basic nutrition guidelines, don’t blame the kidneys. blame the fast food.
Peter Ronai
December 25, 2025 AT 21:18you’re all wrong. the real problem is pharmaceutical companies pushing low-protein diets so they can sell more meds. this whole thing is a scam. i’ve read 47 papers on this. none of you have.
Brooks Beveridge
December 27, 2025 AT 09:54you’re doing amazing just by seeking info 💙
start with one swap this week - maybe swap soda for sparkling water with lemon. small wins add up. i’m rooting for you!
Sachin Bhorde
December 28, 2025 AT 16:07stage 3? go for 0.6g/kg but make sure ur protein is high biological value - eggs, whey, milk. avoid plant proteins if u have acidosis. also, check ur potassium. too many ppl forget that.
Joe Bartlett
December 30, 2025 AT 09:46my mate in london went from stage 4 to stage 3 just by eating more eggs and less bread. no meds. just food. proof it works.