SGLT2 Inhibitors and Fournier’s Gangrene: What to Watch For and What to Do
 Dec, 1 2025
Dec, 1 2025
Fournier's Gangrene Risk Assessment Tool
Critical Warning
Fournier's gangrene is a medical emergency. If you're taking an SGLT2 inhibitor and experience any symptoms, act immediately. Every hour of delay increases death risk by 9%. Go to the emergency room now.
When you’re managing type 2 diabetes, taking an SGLT2 inhibitor like canagliflozin, dapagliflozin, empagliflozin, or ertugliflozin can be a game-changer. These drugs help lower blood sugar by making your kidneys flush out excess glucose through urine. But there’s a rare, serious risk tied to them that most people never hear about until it’s too late: Fournier’s gangrene.
This isn’t a common side effect. In fact, it happens in fewer than 2 out of every 100,000 people taking these medications each year. But when it does happen, it moves fast-and it can kill. That’s why knowing the warning signs and acting immediately isn’t just important-it’s life-or-death.
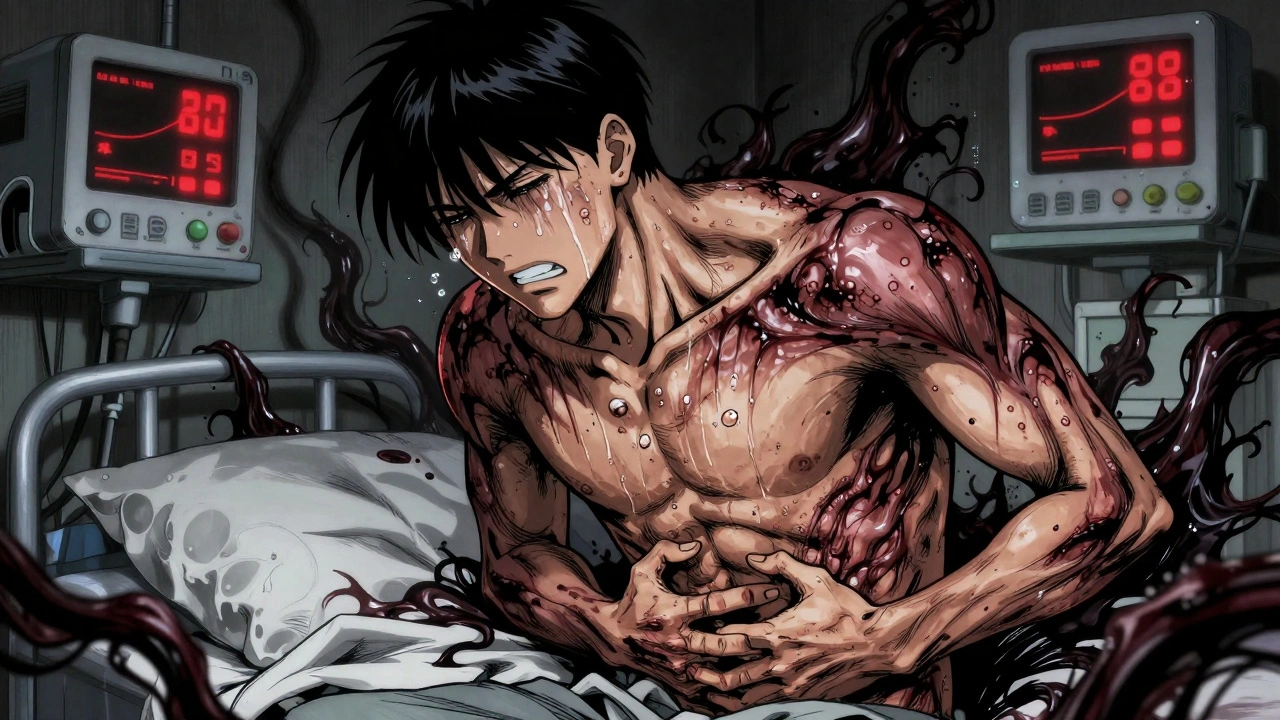
What Is Fournier’s Gangrene?
Fournier’s gangrene is a type of necrotizing fasciitis, a bacterial infection that destroys skin, fat, and the tissue covering muscles. It starts in the genital or anal area and spreads rapidly. The infection eats through tissue, causing it to die. Without urgent treatment, the bacteria can enter the bloodstream and trigger septic shock.
It’s most common in men with diabetes, but it’s not exclusive to them. About one-third of reported cases in Europe involved women. Most patients had poor blood sugar control at the time of onset. But even people with well-managed diabetes aren’t completely safe-especially if they’re taking an SGLT2 inhibitor.
Why Do SGLT2 Inhibitors Increase the Risk?
SGLT2 inhibitors work by blocking glucose reabsorption in the kidneys. That means extra sugar ends up in your urine. Sounds harmless, right? But that sugar becomes a buffet for bacteria.
The moist, sugary environment around the genitals creates the perfect breeding ground for organisms like E. coli, Klebsiella, and anaerobic bacteria. These bugs don’t just sit there-they multiply fast. And when your immune system is already working harder because of diabetes, it’s harder to fight back.
There’s also evidence that glucose in the urine may weaken tissue barriers, making it easier for bacteria to invade deeper layers of skin and muscle. The exact immune effects aren’t fully understood, but the pattern is clear: more urinary glucose = higher risk of this rare but devastating infection.
Early Warning Signs You Can’t Ignore
The biggest mistake people make? Waiting. Fournier’s gangrene doesn’t creep in. It explodes.
If you’re taking an SGLT2 inhibitor and notice any of these symptoms-especially if they come on suddenly-don’t wait. Don’t call your pharmacy. Don’t check Google. Go to the emergency room now:
- Severe pain or tenderness in the genitals, scrotum, or around the anus
- Redness, swelling, or warmth in the area that spreads quickly
- Skin that looks bruised, black, or has a crackling sensation when touched (this is gas from bacteria)
- Fever, chills, or feeling extremely unwell
- Bad-smelling discharge from the genital area
These symptoms can appear within hours. One patient in a 2022 case report went from mild discomfort to needing surgery in less than 12 hours. Another described it as “a burning pain that felt like my groin was on fire.”
Don’t dismiss it as a yeast infection or a pimple. Those can be treated with creams. This needs a hospital.
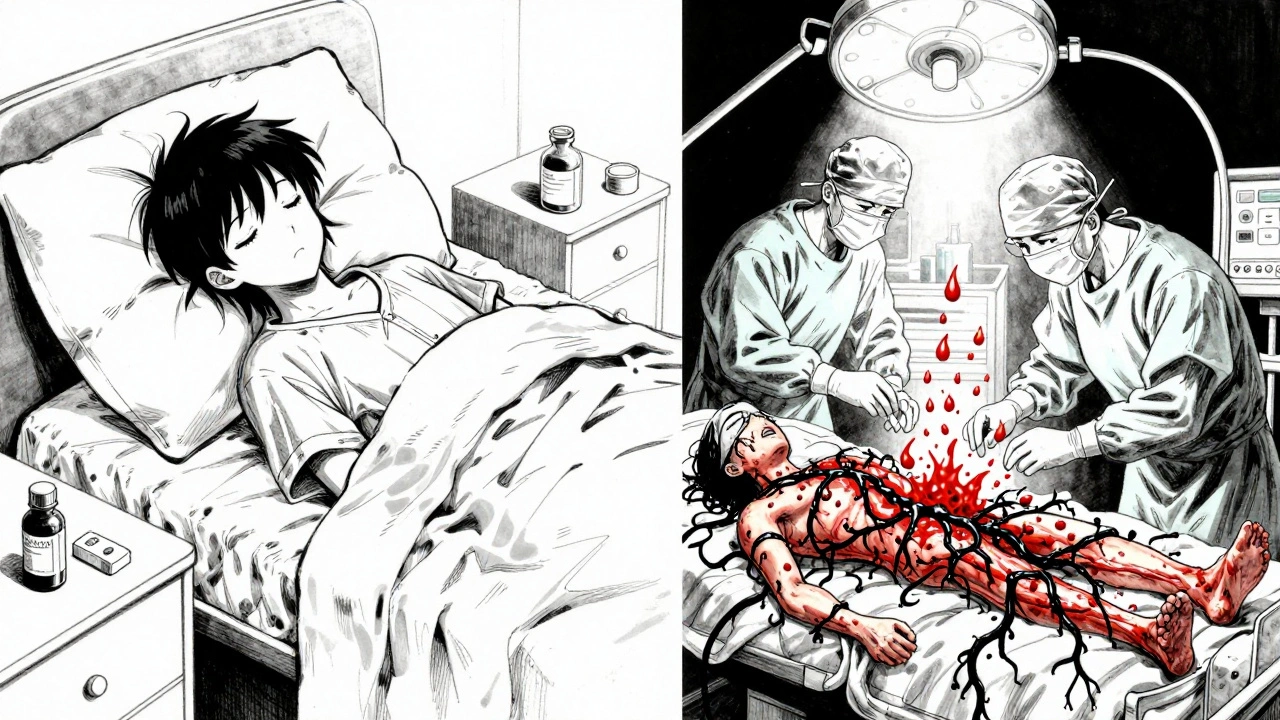
What to Do Immediately
If you suspect Fournier’s gangrene, here’s what you must do:
- Stop taking your SGLT2 inhibitor. Don’t wait for your doctor’s call. Discontinue it right away.
- Call 999 or go to the nearest emergency department. Tell them you’re on an SGLT2 inhibitor and suspect Fournier’s gangrene. Use those exact words.
- Do not delay. Every hour without treatment increases your risk of death by about 9%. Surgery within 24 hours improves survival chances dramatically.
At the hospital, you’ll likely get broad-spectrum antibiotics right away and be taken to surgery for debridement-removing dead tissue. Sometimes multiple surgeries are needed. Recovery takes weeks or months, and scarring or reconstructive surgery may follow.
Survival rates are better than they used to be-around 92% if treated within 24 hours. But if you wait 48 hours or longer, the death rate jumps to nearly 40%.
Who’s at Higher Risk?
Not everyone on SGLT2 inhibitors needs to panic. But certain people should be extra cautious:
- Men with diabetes (though women are also at risk)
- People with HbA1c over 9%-poor blood sugar control is a major factor
- Those who’ve had recurrent genital yeast infections or urinary tract infections
- People with weakened immune systems (due to steroids, chemotherapy, or other conditions)
- Those with obesity or poor hygiene practices
Even if you fit one or more of these categories, that doesn’t mean you should stop your medication. The benefits of SGLT2 inhibitors-lowering heart failure risk, protecting your kidneys, and helping you lose weight-often outweigh the risk of this rare complication.
But you need to be informed. Talk to your doctor before starting the drug. Ask: “What should I watch for?” and “What do I do if I notice something strange?”
Regulatory Warnings and What They Mean
In 2018, the U.S. FDA added a boxed warning to all SGLT2 inhibitors-the strongest type of safety alert. The European Medicines Agency and the UK’s MHRA followed suit. These aren’t just footnotes. They’re red flags.
As of 2024, the FDA has documented over 100 cases linked to these drugs since 2013. The UK reported 6 cases between 2013 and early 2019, with 4 in men and 2 in women. That’s not a lot-but it’s enough to change how doctors prescribe.
Pharmacists now routinely hand out patient leaflets that list Fournier’s gangrene as a possible side effect. Doctors are trained to discuss it during the first visit. But patients still miss it. That’s why you need to know the signs yourself.
What About the Benefits?
Let’s be clear: SGLT2 inhibitors save lives. They reduce hospitalizations for heart failure by up to 30% in high-risk patients. They slow kidney disease progression-even in people without diabetes. For many, they’re the best tool they’ve had.
The risk of Fournier’s gangrene is real, but it’s rare. The risk of a heart attack or stroke from uncontrolled diabetes? Much higher.
Don’t stop your medication out of fear. Stop it only if you see the signs. And if you’re unsure, talk to your doctor. They can help you weigh your personal risks.
What’s Next?
Researchers are working on tools to better predict who’s most at risk. Future guidelines may include checking for prior genital infections or HbA1c levels before prescribing. For now, the best defense is awareness.
If you’re on an SGLT2 inhibitor, keep a mental checklist: pain, redness, swelling, fever. If any show up, act fast. Your life depends on it.
Most people take these drugs safely for years. But for the few who develop this infection, timing is everything. Know the signs. Trust your body. And never wait to get help.
Can women get Fournier’s gangrene from SGLT2 inhibitors?
Yes. While Fournier’s gangrene is more common in men, about one-third of reported cases in Europe involved women. Any person taking an SGLT2 inhibitor who notices sudden pain, swelling, or redness in the genital or perineal area should seek emergency care, regardless of gender.
Is Fournier’s gangrene the same as a yeast infection?
No. Yeast infections cause itching, discharge, and mild discomfort. Fournier’s gangrene causes intense pain, rapid swelling, fever, and skin that turns dark or feels crackly. Yeast infections respond to antifungal creams. Fournier’s gangrene requires emergency surgery and antibiotics. If symptoms are worsening quickly, treat it as an emergency.
Should I stop taking my SGLT2 inhibitor if I’m worried?
No-not unless you have symptoms. Stopping the drug without medical advice can cause your blood sugar to spike, increasing your risk of heart and kidney problems. The risk of Fournier’s gangrene is very low. Focus on knowing the warning signs instead. If you’re concerned, talk to your doctor about your personal risk factors.
How soon should I go to the hospital if I suspect Fournier’s gangrene?
Immediately. Every hour of delay increases your risk of death by about 9%. Do not wait until morning. Do not call your GP first. Go straight to the emergency department and tell them you’re on an SGLT2 inhibitor and suspect Fournier’s gangrene. Speed saves lives.
Are all SGLT2 inhibitors equally risky?
Yes. The risk appears to be a class effect, meaning all drugs in this group-canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin-carry the same potential risk. The mechanism (glucose in urine) is the same for all. Regulatory agencies have issued warnings for the entire class.
Can I get Fournier’s gangrene even if my diabetes is well-controlled?
Yes, but the risk is lower. Most cases occur in people with HbA1c over 9%, but even those with good control have been affected. The SGLT2 inhibitor itself creates a bacterial-friendly environment in the urinary tract, regardless of overall blood sugar. That’s why awareness is key for everyone on these drugs.
What happens if I ignore the symptoms?
The infection spreads rapidly, destroying tissue and entering the bloodstream. This leads to septic shock, organ failure, and death. Survivors often face long hospital stays, multiple surgeries, and permanent changes to their anatomy. Delaying treatment is the single biggest factor in poor outcomes.
Will my doctor tell me about this risk?
Many do, but not all. Studies show that patient education on this specific risk is inconsistent. Don’t rely on your doctor bringing it up. Ask: “What are the rare but serious side effects of this drug?” and specifically mention Fournier’s gangrene. If they don’t know, ask for a referral to a diabetes educator.

Lydia Zhang
December 2, 2025 AT 17:53Kay Lam
December 4, 2025 AT 03:42Irving Steinberg
December 5, 2025 AT 21:51Jack Arscott
December 6, 2025 AT 07:47Priyam Tomar
December 6, 2025 AT 12:17Matt Dean
December 7, 2025 AT 02:08Walker Alvey
December 7, 2025 AT 02:23Jaswinder Singh
December 8, 2025 AT 17:03Jeremy Butler
December 8, 2025 AT 17:19Courtney Co
December 10, 2025 AT 07:00Shashank Vira
December 10, 2025 AT 14:33