Sick Euthyroid Syndrome: How Illness Skews Thyroid Lab Results
 Dec, 15 2025
Dec, 15 2025
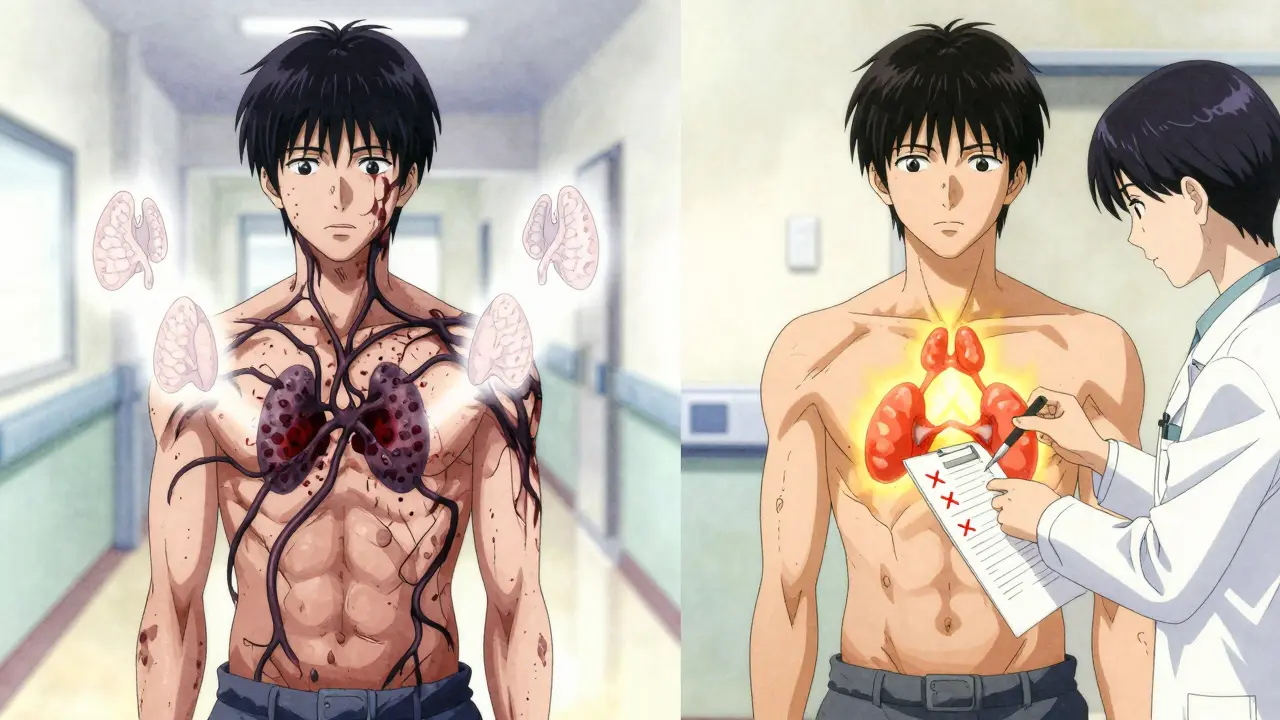
What Is Sick Euthyroid Syndrome?
When you're seriously ill, your body doesn't just feel tired-it changes how it uses energy. One of the quietest, most misunderstood shifts happens in your thyroid hormone levels. Sick euthyroid syndrome (also called nonthyroidal illness syndrome or NTIS) is when your thyroid blood tests look wrong, but your thyroid gland is perfectly fine. It’s not a disease. It’s your body adapting.
This isn’t rare. In intensive care units, 70 to 75% of critically ill patients show these abnormal thyroid numbers. You might see low T3, low T4, high reverse T3, and a TSH that’s normal or just slightly off. To someone unfamiliar, it looks like hypothyroidism. But it’s not. Giving thyroid hormone here won’t help-and it might hurt.
How Illness Changes Your Thyroid Numbers
Your thyroid makes two main hormones: T4 (thyroxine) and T3 (triiodothyronine). T3 is the active form your cells use. Normally, your body converts T4 into T3 as needed. But when you’re sick-whether from infection, trauma, or major surgery-this conversion slows down.
Here’s what actually happens in your blood:
- T3 drops in 95% of cases. This is the most consistent sign.
- T4 drops in about half of severe cases.
- Reverse T3 (rT3) rises-up to 90% of patients. This is an inactive form of T3 that blocks the active one.
- TSH stays normal in most people (60-70%), or dips slightly. It rarely spikes high like in true hypothyroidism.
Why? Your body shuts down the enzyme (type 1 deiodinase) that turns T4 into T3. At the same time, inflammation spikes. Cytokines like IL-6 and TNF-alpha-raised 10 to 15 times higher during sepsis-tell your brain to dial back thyroid activity. It’s not broken. It’s conserving energy.
What Illnesses Trigger This?
Sick euthyroid syndrome doesn’t show up with a cold or the flu. It’s tied to serious, systemic stress:
- Sepsis - affects 80-85% of patients
- Major surgery - seen in 65-70%
- Severe burns - 75-80% of cases
- Heart attack - 50-55%
- Diabetic ketoacidosis - 60-65%
- Chronic conditions like liver cirrhosis (70-75%), kidney failure (60-65%), and anorexia nervosa (up to 90% in severe cases)
Changes can show up in as little as 24 to 48 hours after the illness starts. That’s why labs drawn early in ICU admission often look confusing.
Why It’s Mistaken for Hypothyroidism
The symptoms overlap almost perfectly: fatigue, weakness, feeling cold, constipation, low mood. In fact, 85% of patients with sick euthyroid syndrome report fatigue. But here’s the key difference: they don’t have the physical signs of true hypothyroidism.
No puffy face. No dry skin. No thickened tongue. No myxedema. No elevated thyroid antibodies. No goiter. If your TSH is normal or only mildly low, and your T3 is down, it’s almost certainly not your thyroid.
But doctors sometimes miss this. A 2021 study of 3,200 ICU patients found that 12% got unnecessary thyroid hormone treatment because their labs were misread. And that’s dangerous. Giving levothyroxine to someone with sick euthyroid syndrome doesn’t improve survival. It doesn’t shorten ICU stays. In fact, it may raise the risk of heart rhythm problems and increase mortality by 8-10%.
What Doctors Should Do (and Not Do)
The rule is simple: treat the illness, not the labs.
Don’t start thyroid medication just because T3 is low. Don’t order thyroid tests routinely in ICU patients without clear signs of thyroid disease. The Endocrine Society’s 2022 guidelines say it clearly: 90% of abnormal thyroid tests in critically ill patients are due to sick euthyroid syndrome.
Here’s what works:
- Focus on the root cause-antibiotics for sepsis, fluid resuscitation for shock, glucose control for DKA.
- Wait to check thyroid levels again after recovery. If levels stay abnormal after 4-6 weeks, then investigate for true thyroid disease.
- Look at the full picture. A low TSH with low T3 and T4? That’s central hypothyroidism-rare, but real, and it needs treatment.
- Don’t panic over a mildly high TSH during recovery. It’s often just the thyroid coming back online.
A 2022 trial with 450 ICU patients compared those given levothyroxine to those given placebo. The results? Identical death rates. Identical ICU stays. No benefit. Zero.

Is There Any Value in Monitoring These Levels?
Yes-but not for treatment. For prognosis.
Studies show that the deeper the drop in T3, the higher the risk of dying. Patients with T3 below 40 ng/dL have a 45% mortality rate. Those with T3 above 80 ng/dL? Only 15%. That’s why some ICUs now track T3 trends as a warning sign, not a treatment target.
Researchers are now running large trials, like the EUTHYROID-ICU study, to see if specific patterns in thyroid hormones can predict who will recover and who won’t. If we can use these numbers as a clue-not a diagnosis-we might save more lives.
What Should You Do If You’re Diagnosed?
If you’re in the hospital and your thyroid tests look abnormal, ask: "Is this my thyroid, or is this my illness?"
Don’t push for thyroid meds. Don’t assume you need lifelong treatment. Most people return to normal thyroid function within weeks after they recover. If you’re discharged and still feel tired, give yourself time. Your body has been through a war.
If you’re still having symptoms six weeks later, then see an endocrinologist. But don’t let a single lab result from your ICU stay define your health long-term.
The Bigger Picture
Sick euthyroid syndrome is a reminder that your body is smarter than any lab test. It doesn’t malfunction under stress-it adapts. Slowing metabolism, reducing heat production, conserving energy-these aren’t signs of failure. They’re survival strategies.
Medicine has a habit of pathologizing adaptation. We see a low number, we reach for a pill. But sometimes, the body knows best. The goal isn’t to fix the lab values. It’s to fix the illness. And when you do, the thyroid usually fixes itself.

Himmat Singh
December 16, 2025 AT 23:19While the article presents a compelling clinical narrative, one must not overlook the epistemological limitations inherent in interpreting biomarkers within the context of systemic stress. The conflation of homeostatic adaptation with pathological dysfunction reflects a broader reductionist tendency in modern medicine, wherein physiological responses are pathologized rather than contextualized. The data presented, while statistically significant, lacks ontological grounding in the lived experience of the patient.
Alvin Montanez
December 18, 2025 AT 11:50Let me be absolutely clear here-this whole sick euthyroid syndrome thing is just another example of doctors being too lazy to actually diagnose properly. You see a low T3? You see a low T4? You see reverse T3 climbing like it’s trying to escape the lab report? That’s not ‘adaptation,’ that’s a thyroid that’s failing, and someone’s too scared to admit it. The fact that 12% of ICU patients get unnecessary hormone treatment means 88% are being left to suffer because of this ‘don’t treat the labs’ dogma. Who’s keeping track of how many people are still exhausted six months after they get out of the hospital because their thyroid was never allowed to recover? The Endocrine Society’s guidelines? Please. They’re written by people who’ve never held a dying patient’s hand at 3 a.m. This isn’t conservation-it’s abandonment dressed up as science.
Lara Tobin
December 20, 2025 AT 06:43This made me cry a little, honestly. 😔 I had this happen after my sepsis-my doctors kept talking about levothyroxine, and I just kept saying, ‘I don’t feel like I have hypothyroidism, I feel like I’ve been through hell.’ Thank you for saying what I couldn’t: it’s not broken, it’s healing. I’m still tired sometimes, but I’m alive. And that’s enough for now.
Jamie Clark
December 21, 2025 AT 04:06You think this is about thyroid labs? No. This is about power. Medicine doesn’t want to admit that the body knows how to heal itself better than any pill can force it to. The pharmaceutical industry profits from treating symptoms, not restoring function. Sick euthyroid syndrome is a threat to the entire endocrine industrial complex-because if you stop treating the lab values, you stop selling drugs. And if you stop selling drugs, you stop funding research, you stop funding conferences, you stop funding the whole goddamn machine. They don’t want you to know this because if you did, you’d stop trusting them. The body doesn’t malfunction under stress-it reorganizes. And that’s terrifying to people who need control to feel safe.
Keasha Trawick
December 22, 2025 AT 01:43Okay, let’s get wild for a second-this isn’t just ‘sick euthyroid syndrome,’ this is your body going full biohacker mode. T3 down? That’s your mitochondria hitting pause. rT3 up? That’s your cells putting up a ‘do not disturb’ sign on the energy switchboard. Cytokines screaming like a rave DJ? That’s your immune system throwing a party and your thyroid’s like, ‘I’m not dancing tonight, I’m on cleanup duty.’ This isn’t disease-it’s a metabolic ninja move. Your body isn’t broken, it’s in stealth mode. And if you give it T4, you’re basically handing it a Starbucks while it’s trying to meditate in a warzone. The real magic? When you stop treating the numbers and start treating the *story*-that’s when the magic happens. The thyroid doesn’t need a pill. It needs peace.
Bruno Janssen
December 23, 2025 AT 15:59I read this in the ICU waiting room. My mom’s on a ventilator. They said her T3 is low. I didn’t say anything. I just stared at the numbers. I don’t know if this is good or bad. I just want her to wake up.
Scott Butler
December 23, 2025 AT 18:25Why are we letting foreign medical guidelines dictate how we treat American patients? The Endocrine Society is full of Ivy League ivory tower types who’ve never seen a real ICU. We’ve got real doctors here who know what’s what-low T3 means low thyroid. Period. No more ‘adaptation’ nonsense. We need American-made protocols, not European-style wishy-washy ‘wait and see’ nonsense. Our soldiers, our firefighters, our nurses-they don’t get to wait six weeks to feel better. They need treatment now. Stop letting bureaucrats decide who lives and who dies.
Emma Sbarge
December 24, 2025 AT 02:32I’ve worked in ICUs for 22 years. I’ve seen this a thousand times. The lab numbers lie. The patient doesn’t. I’ve had patients with T3 at 38 ng/dL who were walking out the door two weeks later like nothing happened. And I’ve had patients with perfect labs who never woke up. It’s never about the numbers. It’s about the person. If you’re treating the lab, you’re not treating the patient. And if you’re not treating the patient, you’re not a doctor-you’re a data entry clerk with a stethoscope.
Deborah Andrich
December 24, 2025 AT 07:27Thank you for writing this. I’ve been trying to explain this to my sister since she came home from the hospital last year. She’s still tired, and her doctor keeps saying ‘your thyroid’s fine now’ like that’s supposed to make her feel better. But it’s not about the thyroid. It’s about the war she fought inside her body. And wars don’t end when the battle stops-they end when the body finally stops holding its breath. We need to stop treating recovery like a checkbox and start treating it like a slow, sacred return. You don’t fix a soul with a pill. You give it time. And quiet. And care. That’s all.
Jennifer Taylor
December 24, 2025 AT 16:19Wait-this is all a cover-up for Big Pharma’s real agenda. Did you know the FDA approved synthetic T3 in 1998? That’s the same year the WHO declared thyroid disorders a global health priority. Coincidence? I think not. Reverse T3? That’s not a byproduct-it’s a marker. And the markers are being manipulated. The truth? They’re using sick euthyroid syndrome to hide the fact that glyphosate and EMF radiation are wrecking our mitochondria. Your thyroid isn’t adapting-it’s being poisoned. And they don’t want you to know. They want you to believe it’s ‘just stress.’ But it’s not. It’s a silent genocide. Wake up.
Shelby Ume
December 25, 2025 AT 02:09As a clinical educator, I’ve trained dozens of residents on this exact topic. The most dangerous misconception isn’t that we over-treat-it’s that we assume patients understand the difference between ‘abnormal’ and ‘pathological.’ We hand them a lab report with arrows pointing down and say, ‘You’re hypothyroid.’ We don’t say, ‘Your body is conserving energy because it’s fighting for its life.’ We reduce their trauma to a number. And then we wonder why they feel unheard. This isn’t just a medical issue. It’s a communication crisis. We need to teach our students to speak to patients as humans-not as data points.