Stroke Types and Causes Explained
 Oct, 15 2025
Oct, 15 2025
Stroke Risk Assessment Tool
Stroke Risk Assessment
This tool estimates your relative risk of stroke based on key medical factors and lifestyle habits. Results are for informational purposes only and do not replace professional medical advice.
Your Risk Factors
When a blood vessel in the brain suddenly stops delivering oxygen, the result is a stroke is a medical emergency caused by disruption of blood flow to brain tissue. Within minutes, brain cells can begin to die, making rapid recognition and treatment vital.
stroke types differ in mechanism and treatment, so knowing them helps you act faster.
Quick Takeaways
- Strokes fall mainly into two categories: ischemic (blockage) and hemorrhagic (bleeding).
- Transient ischemic attacks (TIAs) are warning signs that often precede a full‑blown stroke.
- High blood pressure, smoking, and atrial fibrillation top the list of modifiable risk factors.
- Symptoms usually appear suddenly: facial droop, arm weakness, speech trouble - remember “FAST”.
- Early treatment, especially for ischemic stroke, can drastically improve outcomes.
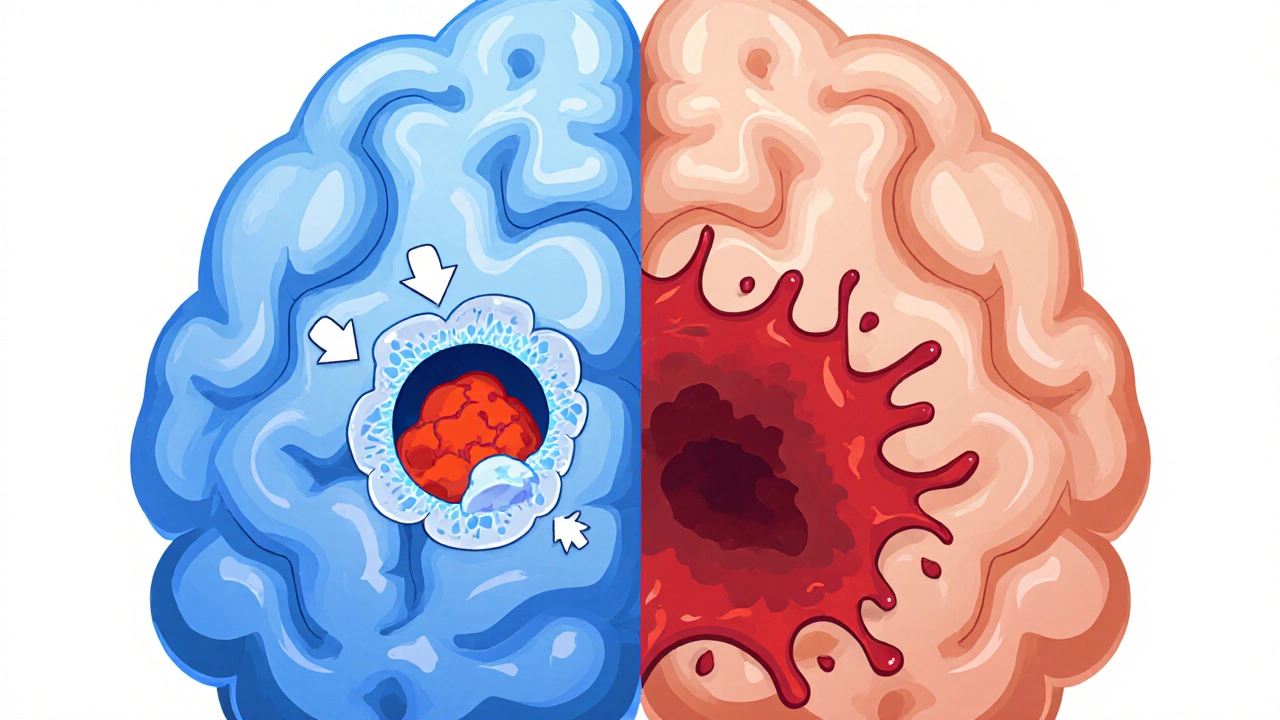
Major Types of Strokes
Ischemic stroke accounts for roughly 85 % of all strokes. It occurs when a clot or a narrowed artery blocks blood flow.
Thrombotic stroke
A thrombotic stroke develops from a blood clot that forms directly inside a brain artery, often on a plaque‑filled vessel. It typically progresses slowly, giving a brief warning before the full event.
Embolic stroke
An embolic stroke occurs when a clot travels from elsewhere in the body, such as the heart, and lodges in a cerebral artery. Atrial fibrillation is a common source of these traveling clots.
Transient ischemic attack (TIA)
Often called a “mini‑stroke,” a transient ischemic attack lasts only minutes and leaves no permanent damage. It’s a crucial warning sign; up to 1 in 3 people having a TIA will suffer a full stroke within a year if risk factors aren’t addressed.
Hemorrhagic stroke makes up the remaining 15 % and involves bleeding inside or around the brain.
Intracerebral hemorrhage
An intracerebral hemorrhage is bleeding directly into the brain tissue, often caused by uncontrolled hypertension. It can expand quickly, raising intracranial pressure.
Subarachnoid hemorrhage
A subarachnoid hemorrhage occurs when blood collects in the space between the brain and its protective membrane, frequently following a ruptured aneurysm. Sudden “thunderclap” headache is a hallmark symptom.
Key Causes and Risk Factors
Understanding what leads to a stroke helps you control it. The main risk factors are conditions or habits that increase the likelihood of a stroke include:
- High blood pressure: The single biggest preventable cause; each 10 mmHg rise doubles stroke risk.
- Smoking: Damages artery walls and accelerates clot formation.
- Atrial fibrillation: Creates erratic blood flow in the heart, raising embolic stroke chances.
- Diabetes: Elevates blood vessel damage, promoting both ischemic and hemorrhagic events.
- High cholesterol: Leads to plaque buildup, narrowing arteries.
- Excessive alcohol, sedentary lifestyle, and obesity also contribute significantly.
How Ischemic and Hemorrhagic Strokes Differ
| Feature | Ischemic Stroke | Hemorrhagic Stroke |
|---|---|---|
| Primary cause | Blocked blood vessel (thrombus or embolus) | Bleeding into brain tissue or surrounding space |
| Typical risk factors | High cholesterol, atrial fibrillation, diabetes | Uncontrolled hypertension, aneurysm, anticoagulant use |
| Onset speed | Often sudden but may develop over minutes | Very rapid, can deteriorate within hours |
| Treatment focus | Restore flow (clot‑busting drugs, mechanical thrombectomy) | Control bleeding, reduce pressure (surgery, blood‑pressure management) |
| Mortality rate | ~10 % (varies with severity) | ~40 % (higher for subarachnoid hemorrhage) |
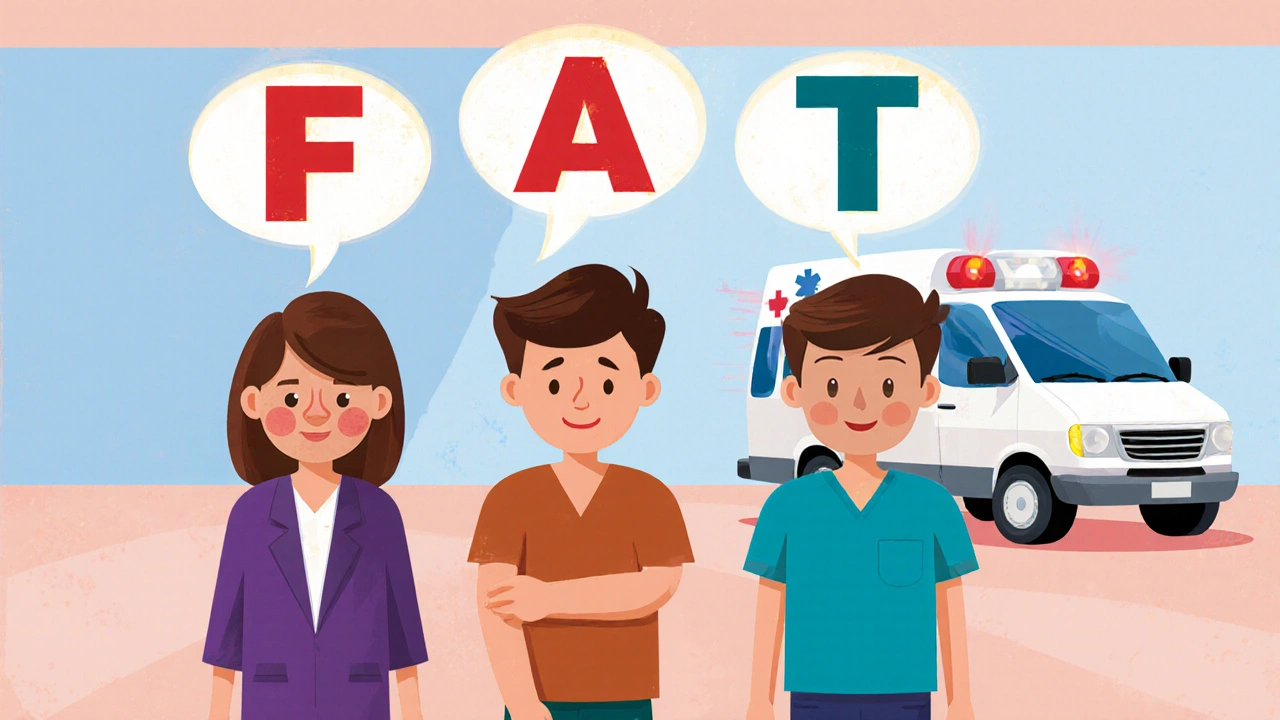
Recognizing the Warning Signs
Time is brain. The FAST acronym helps you act fast:
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call emergency services
Other clues include sudden vision loss, severe headache, loss of balance, or confusion. If you suspect a stroke, call emergency services immediately - every minute saved can preserve up to 1.9 million neurons.
Prevention Strategies You Can Implement Today
- Monitor blood pressure regularly; aim for <130/80 mmHg.
- Quit smoking; use nicotine replacement or counseling if needed.
- Manage atrial fibrillation with anticoagulants as prescribed.
- Adopt a Mediterranean‑style diet rich in fruits, vegetables, whole grains, and omega‑3 fatty acids.
- Stay active - at least 150 minutes of moderate aerobic exercise per week.
- Limit alcohol to ≤2 drinks per day for men, ≤1 for women.
Next Steps After a Stroke Diagnosis
Recovery continues beyond the hospital. A multidisciplinary approach - neurologist, physiotherapist, speech therapist, and dietitian - improves functional outcomes. Participate in cardiac rehab‑style programs, track progress, and adjust risk‑factor management as needed.
Frequently Asked Questions
Can a TIA be treated the same way as a full stroke?
TIAs don’t require clot‑busting drugs because they resolve on their own, but they trigger urgent evaluation and preventive treatment (e.g., antiplatelet therapy, blood‑pressure control) to stop a future stroke.
Why are hemorrhagic strokes more deadly?
Bleeding raises intracranial pressure quickly, compressing vital brain structures. Surgical options are limited, and the underlying cause (often uncontrolled hypertension) can be hard to reverse in the acute phase.
Is there a genetic component to stroke risk?
Family history matters, especially for conditions like atrial fibrillation, high cholesterol, and intracranial aneurysms. Genetic testing can identify at‑risk relatives, prompting earlier screening.
How quickly must treatment start for an ischemic stroke?
The first 3‑hour window is critical for intravenous thrombolysis; newer guidelines extend it to 4.5 hours in select patients. Mechanical thrombectomy can be effective up to 24 hours after symptom onset for large‑vessel occlusions.
Can lifestyle changes reverse an existing stroke?
While you can’t undo damaged brain tissue, rigorous risk‑factor control and rehabilitation can improve function, reduce recurrence, and enhance quality of life.

Amit Kumar
October 15, 2025 AT 13:30Great summary! 😃
Crystal Heim
October 25, 2025 AT 23:30The article covers the basics but lacks depth.
Abhimanyu Singh Rathore
November 4, 2025 AT 04:44Wow, what an exhaustive rundown, from ischemic to hemorrhagic, from risk factors to FAST, every detail is presented with clarity, and the table really helps compare the two major types, kudos to the author for such a thorough piece!
Stephen Lewis
November 12, 2025 AT 07:10While the composition is commendable in its breadth, one might consider integrating recent guidelines from the American Heart Association to further enhance its clinical relevance.
janvi patel
November 19, 2025 AT 05:50Although the facts are correct, the presentation feels overly didactic and could benefit from a more engaging narrative style.
Lynn Kline
November 25, 2025 AT 00:44This guide is a brilliant tapestry of information-vivid, precise, and undeniably useful; the way it demystifies the FAST acronym alone is a masterstroke, and the inclusion of lifestyle tips adds that extra sparkle!
Rin Jan
November 29, 2025 AT 15:50Strokes are not merely medical jargon; they represent a profound disruption of the brain's lifeline.
When a vessel congeals or bursts, countless neurons are left scrambling for oxygen that will never arrive.
The cascade that follows is relentless, leading to irreversible damage if intervention is delayed.
Therefore, recognizing the subtle signs before the full-blown event can be the difference between life and lasting disability.
The transient ischemic attack, often dismissed as a minor inconvenience, is in fact a stark warning bell.
Ignoring that signal is akin to ignoring a fire alarm in a crowded building.
High blood pressure, the silent assassin, gnaws at arterial walls, paving the way for both clot formation and hemorrhage.
Smoking compounds the risk by poisoning the endothelium and accelerating atherosclerosis.
Atrial fibrillation, an erratic heartbeat, serves as a rogue ferry transporting clots to the brain's delicate vasculature.
Diabetes, through its relentless assault on small vessels, further destabilizes cerebral circulation.
The synergy of these factors creates a perfect storm, one that can be mitigated through disciplined lifestyle changes.
Regular monitoring of blood pressure, quitting tobacco, maintaining a balanced diet, and staying physically active are not mere recommendations; they are imperatives.
Moreover, timely medical therapy-such as clot-busting agents for ischemic strokes-can restore perfusion and salvage compromised tissue.
Conversely, hemorrhagic strokes demand rapid blood pressure control and, in some cases, surgical decompression.
The ultimate goal is simple: preserve as many neurons as possible, because each one contributes to the mosaic of our thoughts, emotions, and abilities.
In sum, awareness, prevention, and swift action form the trifecta that can turn a potential tragedy into a manageable event.
Jessica Taranto
December 3, 2025 AT 03:10I completely agree with the emphasis on prevention; regularly checking blood pressure and reducing smoking are indeed crucial steps.
akash chaudhary
December 6, 2025 AT 00:37While the prose is colorful, the article omits recent data on the efficacy of mechanical thrombectomy, which is a glaring oversight.
kenneth strachan
December 8, 2025 AT 08:10Honestly, this read felt like a snoozefest; where's the real-life patient story that makes the stakes tangible?
Mandy Mehalko
December 10, 2025 AT 01:50The practical tips at the end are super helpful-thanks for including them!
Bryan Kopp
December 11, 2025 AT 11:10Your critique overlooks the human element; many readers rely on this clear guidance to recognize a stroke in time.
Patrick Vande Ven
December 12, 2025 AT 14:57From a statistical standpoint, the mortality differential between ischemic and hemorrhagic strokes aligns with established epidemiological trends.
Tim Giles
December 13, 2025 AT 13:10The intricate pathophysiology behind clot formation involves a cascade of platelet activation, fibrin deposition, and endothelial dysfunction; understanding these mechanisms can inform both prophylactic and acute therapeutic strategies. Additionally, emerging biomarkers such as neurofilament light chain show promise in early detection, although further validation is required. Moreover, one must consider the socioeconomic determinants that influence access to timely care, as disparities persist across regions. Finally, continuous education of both clinicians and the public remains the cornerstone of reducing stroke burden.
Peter Jones
December 14, 2025 AT 05:50Let's remember that sharing accurate information empowers everyone, and constructive dialogue only strengthens our collective knowledge.
Scott Davis
December 14, 2025 AT 19:44Spot on.