Vaginal Surgery FAQs: Common Questions Answered
 Oct, 12 2025
Oct, 12 2025
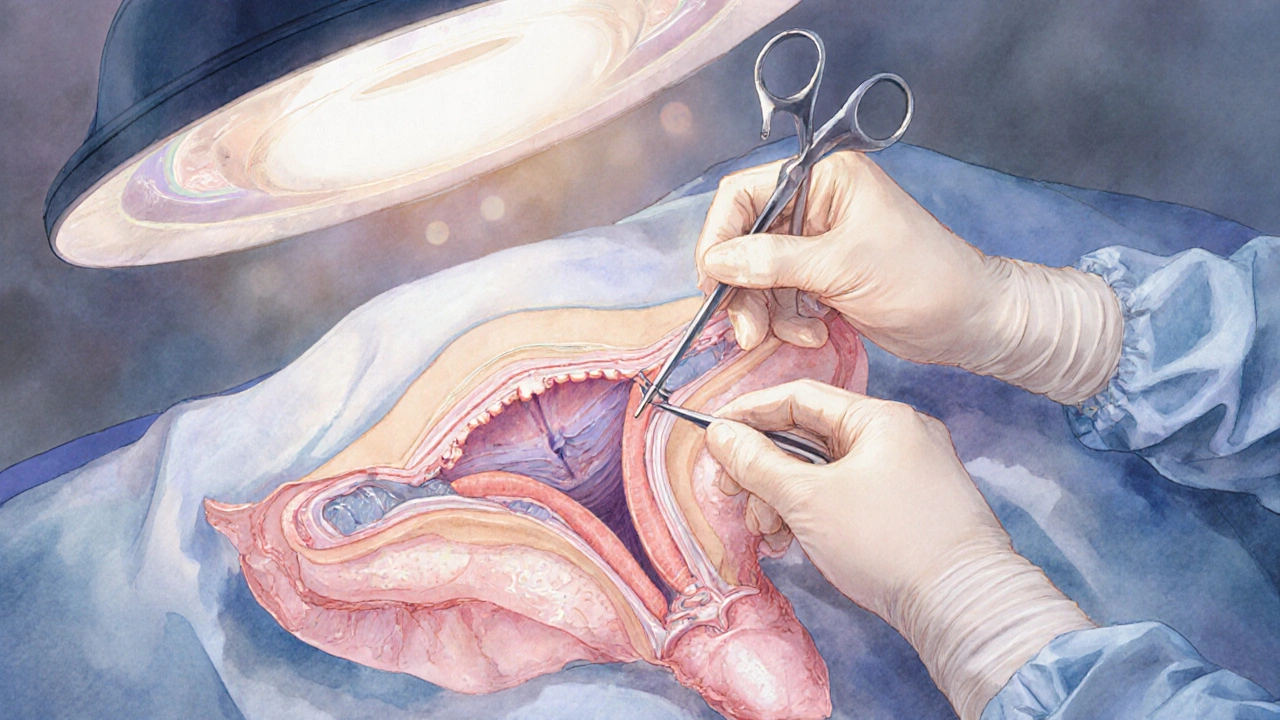
Ever wondered what really happens when a doctor operates on the vagina? Vaginal surgery can sound intimidating, but most patients just want clear answers about why it’s needed, how it works, and what the road to recovery looks like. Below we break down the most common queries, from the basics of the procedure to the nitty‑gritty of postoperative care.
Key Takeaways
- Vaginal surgery includes a range of procedures, each targeting a specific issue such as prolapse, cosmetic concerns, or functional problems.
- Pre‑op evaluation focuses on overall health, pelvic anatomy, and patient goals.
- Most surgeries are done under regional or general anesthesia with same‑day discharge for minor cases.
- Recovery typically spans 4-6 weeks for full healing, but daily activities may resume sooner.
- Understanding risks - infection, bleeding, and changes in sexual or urinary function - helps set realistic expectations.
What Is Vaginal Surgery?
Vaginal Surgery is a collective term for any operative procedure performed through the vaginal canal, aiming to repair, reconstruct, or enhance vaginal tissues. It can address medical conditions like pelvic organ prolapse, address congenital or acquired structural issues, or fulfill aesthetic goals. Unlike abdominal approaches, the vaginal route often results in less postoperative pain, shorter hospital stays, and faster return to normal activities.
Common Types of Vaginal Surgery
Below is a snapshot of the most frequently performed procedures, each with its own purpose and typical recovery timeline.
| Procedure | Primary Indication | Typical Recovery | Key Risks |
|---|---|---|---|
| Labiaplasty | Excess labial tissue causing discomfort or cosmetic concerns | 2-3 weeks for daily activities | Infection, altered sensation |
| Vaginal Reconstruction | Severe vaginal shortening or scarring after trauma or cancer treatment | 4-6 weeks for full healing | Scar formation, dyspareunia |
| Pelvic Organ Prolapse Repair (via vagina) | Descent of bladder, uterus, or rectum into the vagina | 4-8 weeks for full activity | Recurrence, urinary issues |
| Hymenoplasty | Cultural or personal desire to restore an intact hymen | 1-2 weeks for light activity | Bleeding, infection |
| Vaginectomy (partial) | Removal of part of the vaginal wall due to cancer or severe disease | 6-12 weeks for complete healing | Fistula formation, sexual dysfunction |
When Is Vaginal Surgery Recommended?
Doctors consider surgery after conservative measures fail or when the condition poses a health risk. Typical triggers include:
- Persistent pelvic organ prolapse causing urinary leakage, bowel problems, or chronic pressure.
- Significant labial hypertrophy leading to irritation, chafing, or difficulty with clothing.
- Scar tissue after radiation therapy that narrows the vaginal canal, impacting intercourse or examinations.
- Patient‑driven cosmetic goals, provided the benefits outweigh potential complications.
During the pre‑operative visit, a Surgeon will assess pelvic floor strength, review imaging (often an MRI or pelvic ultrasound), and discuss realistic outcomes.
Preparing for Surgery: What to Expect
Preparation helps smooth the operative day and reduces anxiety.
- Medical Clearance: Your primary care physician or a specialist will run blood tests, check heart health, and review any medications that could affect bleeding (like blood thinners).
- Pre‑operative Counseling: A detailed discussion about anesthesia options - most vaginal procedures use regional anesthesia (spinal or epidural) or general anesthesia for longer cases.
- Fasting Guidelines: Usually nothing by mouth after midnight before the surgery, unless a specific protocol says otherwise.
- Hygiene: Patients are instructed to clean the vaginal area with mild soap and avoid vaginal creams or douches for 24 hours before the operation.
- Support System: Arrange for a friend or family member to drive you home and stay for at least the first night.
Ask your Anesthesia team any concerns about pain control or potential allergic reactions to medication.
Recovery and After‑care
Recovery plans differ based on the procedure’s extent, but some universal guidelines apply.
- Pain Management: Doctors prescribe a short course of acetaminophen‑based analgesics, reserving opioids for breakthrough pain. Non‑steroidal anti‑inflammatory drugs (NSAIDs) are avoided if there’s a bleeding risk.
- Activity Restrictions: Light walking is encouraged within the first 24‑48 hours to improve circulation. Heavy lifting, strenuous exercise, and sexual intercourse are usually delayed for 4-6 weeks.
- Wound Care: Keep the incision clean and dry. If sutures are absorbable, no removal is needed; otherwise, a follow‑up visit in 7-10 days will be scheduled.
- Pelvic Floor Exercises: Gentle Kegel exercises can aid healing, but a physiotherapist may recommend a tailored regimen to avoid strain.
- Monitoring for Complications: Watch for fever, excessive bleeding, foul discharge, or new urinary urgency. Promptly contact your clinic if any of these arise.
Most patients feel back to “normal” after about six weeks, though some may experience lingering sensitivity or mild discomfort during intercourse, which often resolves with time and physical therapy.

Risks and Complications
Every surgery carries inherent risks. Understanding them helps you weigh the benefits.
| Risk | Incidence | Typical Management |
|---|---|---|
| Infection | 1‑3% | Antibiotics, wound care |
| Bleeding | 2‑5% | Compression, possible re‑exploration |
| Urinary Retention | 4‑8% | Temporary catheter, pelvic floor retraining |
| Dyspareunia (painful intercourse) | 5‑10% | Lubricants, physiotherapy, possible revision |
| Recurrence of Prolapse | 10‑15% (depending on technique) | Repeat surgery or pessary use |
Most complications are manageable and resolve with appropriate follow‑up. Discuss any personal health concerns-such as diabetes, smoking, or obesity-with your surgeon, as these can increase risk.
Frequently Asked Questions
Below are answers to the queries we hear most often.
Is vaginal surgery painful?
Will I feel pain during the operation?
No. With proper anesthesia-usually a spinal block or general anesthesia-you will be completely unaware of the procedure. Post‑operative pain is typically mild to moderate and well‑controlled with prescribed medication.
How long will I stay in the hospital?
Most minor procedures, like labiaplasty or hymenoplasty, are done on an outpatient basis-meaning you can go home the same day. More extensive reconstructions may require an overnight stay for monitoring.
Can I have children after vaginal surgery?
In most cases, fertility is not affected. However, procedures that involve extensive tissue removal or scarring could potentially impact the birth canal. Discuss future pregnancy plans with your surgeon before deciding.
Will my sexual pleasure change?
Outcomes vary. Many women report improved comfort and confidence, leading to better sexual experiences. A small percentage experience temporary or permanent changes in sensation; this is why a thorough pre‑op discussion about expectations is crucial.
How soon can I return to work?
For desk‑based jobs, many patients resume work within 1‑2 weeks after minor procedures. More physically demanding roles may require 4‑6 weeks of limited activity.
Do I need a catheter after surgery?
A short‑term catheter is common after extensive prolapse repairs to keep the bladder empty while swelling subsides. It’s usually removed within 24‑48 hours.
What follow‑up appointments are required?
Typically, a first visit occurs 7‑10 days post‑op to check wound healing, followed by a 4‑6 week visit to assess functional recovery and address any lingering concerns.
Next Steps If You’re Considering Vaginal Surgery
Start by scheduling a consultation with a board‑certified Gynecologic Surgeon who specializes in vaginal procedures. Bring a list of your symptoms, any previous imaging, and questions about anesthesia, recovery time, and costs. A clear, honest dialogue at this stage sets the foundation for a smooth surgical journey.
Remember, informed decisions empower you to feel confident about your body and health. With the right information and a supportive care team, vaginal surgery can safely address the issues that matter most to you.

Brennan Loveless
October 12, 2025 AT 14:25When you stare at the glossy brochures promising a “quick fix,” it’s easy to forget that every incision is a pact with your own biology. The United States prides itself on cutting‑edge medicine, yet many patients wander in blinded by the hype, assuming that a surgeon can rewrite anatomy without consequence. Think of the pelvis as a finely tuned orchestra; pulling a single string will reverberate through the whole symphony. That’s why a thorough pre‑op evaluation isn’t a bureaucratic hurdle-it’s the conductor’s score. If you’re ready to weigh the benefits against the risks, the first step is honest self‑assessment, not glossy marketing.
Vani Prasanth
October 14, 2025 AT 21:58It’s wonderful to see such openness about these procedures; sharing knowledge empowers women everywhere. Remember to keep a list of all your concerns and bring it to the consultation-nothing is too small. A supportive care team will walk you through each stage, from imaging to postoperative pelvic‑floor exercises. If you feel uneasy, ask for a second opinion; collaborative decision‑making leads to better outcomes.
Maggie Hewitt
October 17, 2025 AT 05:32Oh, absolutely, because nothing says “I love my body” like scheduling a day off just to get a labia trim.
Sure, the recovery is “just a couple of weeks,” as if you’ll be sprinting marathons by day three.
And let’s not forget the joy of explaining to friends why you need a “hymen reboot.”
Mike Brindisi
October 19, 2025 AT 13:05First you get the blood work then the imaging then the anesthesia consult then the surgeon explains the steps then you sign consent forms then you get prepped then the operation happens then you wake up and it hurts a bit then you go home and follow the care plan
Steven Waller
October 21, 2025 AT 20:38Vaginal surgery, while undeniably effective for many conditions, deserves a nuanced discussion that goes beyond the typical FAQ format. First, it is essential to recognize that the vaginal route offers distinct anatomical advantages, such as reduced postoperative pain and shorter hospital stays, when compared with abdominal approaches. Second, patient selection remains paramount; not every individual with prolapse or aesthetic concerns will benefit equally from an operative solution. Third, the pre‑operative work‑up should include a comprehensive pelvic exam, imaging when indicated, and an honest dialogue about functional goals and sexual health expectations. Fourth, anesthesia choices-whether spinal, epidural, or general-must be tailored to the procedure’s length and the patient’s comorbidities. Fifth, the surgeon’s expertise and experience directly influence complication rates, particularly for complex reconstructions. Sixth, postoperative pain management should prioritize multimodal regimens, limiting opioid exposure while ensuring comfort. Seventh, activity restrictions are often misunderstood; light ambulation is encouraged early, whereas heavy lifting and intercourse should be postponed for the recommended 4‑6 weeks. Eighth, vigilant monitoring for early signs of infection, bleeding, or urinary retention can prevent more serious sequelae. Ninth, the role of pelvic‑floor physical therapy cannot be overstated; targeted exercises support tissue healing and functional recovery. Tenth, patients must be aware that certain risks, such as dyspareunia or recurrence of prolapse, may persist despite optimal technique. Eleventh, fertility considerations are generally favorable, yet extensive tissue removal may alter vaginal elasticity, necessitating pre‑conception counseling. Twelfth, cultural and personal values often shape expectations, and clinicians should honor these while providing evidence‑based guidance. Thirteenth, follow‑up schedules typically include an early wound check within 7‑10 days and a more comprehensive evaluation at 4‑6 weeks. Fourteenth, documentation of outcomes, both objective and patient‑reported, contributes to the growing body of literature that refines best practices. Finally, informed consent is not a single event but an ongoing process that empowers patients to make decisions aligned with their health goals and quality‑of‑life aspirations.
Puspendra Dubey
October 24, 2025 AT 04:12Look, sister, the idea of “just a quick fix” is as dramatic as a Bollywood climax-full of glitter but hidden pain. I’ve read a dozen case reports where the “miracle” turned into a nightmare of scar tissue, and the docs barely whisper about it. The pre‑op counseling feels like a whisper in a thunderstorm; you’re left dreaming about a flawless outcome while the surgeon is busy polishing the scalpel. And trust me, the recovery can feel like a monsoon-sweaty, relentless, and you’re stuck in bed wondering if you’ll ever sit on a chair again :) . So, if you’re thinking about it, bring a friend, a journal, and maybe a stash of tea; you’ll need patience more than any suture.
Dany Devos
October 26, 2025 AT 10:45The composition, while comprehensive, neglects to address the psychosocial dimensions that accompany vaginal procedures. A mere enumeration of risks without contextualizing patient anxiety renders the guide insufficient for informed consent. Moreover, the omission of longitudinal data on sexual function undermines its utility for clinicians seeking evidence‑based recommendations.
Sam Matache
October 28, 2025 AT 18:18Let’s dissect the hype: every “new technique” is paraded as a breakthrough, yet the underlying data often hinges on small cohorts and selective reporting. The glossy infographics mask the reality that many of these surgeries are driven by market forces rather than genuine unmet clinical need. If we strip away the marketing veneer, we see a pattern of over‑medicalization that compromises patient autonomy.
Hardy D6000
October 31, 2025 AT 01:52From an American perspective, the emphasis on minimally invasive vaginal approaches aligns with our healthcare system’s drive for cost‑effectiveness and rapid turnover. However, the clinician must remain vigilant that speed does not eclipse safety; rigorous peer‑reviewed protocols are essential to uphold the standards our nation prides itself on.
Patricia Bokern
November 2, 2025 AT 09:25They don’t want you to know the implants are monitored by a shadow network of undisclosed entities.
Darci Gonzalez
November 4, 2025 AT 16:58You’ve got this 😊 keep following the plan and don’t hesitate to call your surgeon if anything feels off
Marcus Edström
November 7, 2025 AT 00:32It’s helpful to create a recovery timeline that balances work responsibilities with gradual activity increase; many find that a step‑by‑step checklist eases anxiety and promotes steady progress.
kevin muhekyi
November 9, 2025 AT 08:05Just a heads‑up, I’ve been through a labiaplasty and the worst part was the awkward first week-easy to get through if you keep the mood light and stick to the basics.
Camille Ramsey
November 11, 2025 AT 15:38Honestly the article’s grammar is a mess-it’s “vagina” not “vaginal” when you’re talking about the organ, and there’s way too many passive‑voice sentences that dilute the important info; clean it up.
Scott Swanson
November 13, 2025 AT 23:12Remember, supportive pep talks are great, but they don’t replace a structured physical‑therapy regimen; if you skip the exercises because “I feel fine,” you’re just setting yourself up for a comeback of the symptoms.
Karen Gizelle
November 16, 2025 AT 06:45It is morally irresponsible to promote surgical alteration as a cosmetic convenience without first addressing the societal pressures that drive women to consider such invasive steps. The culture that equates worth with appearance must be challenged before we celebrate these procedures as simple solutions.
Stephanie Watkins
November 18, 2025 AT 14:18Could you elaborate on which specific pelvic‑floor exercises are most beneficial post‑labial surgery, and how the intensity should be adjusted over the six‑week recovery period?