When to Seek Emergency Care: Red Flags and Symptoms from Medications
 Nov, 14 2025
Nov, 14 2025
Medication Emergency Checker
Check Your Symptoms
Select any symptoms you're experiencing after starting a new medication or changing your dose. This tool helps you determine if your symptoms require emergency medical care.
Select the symptoms you're experiencing to see if you need emergency care.
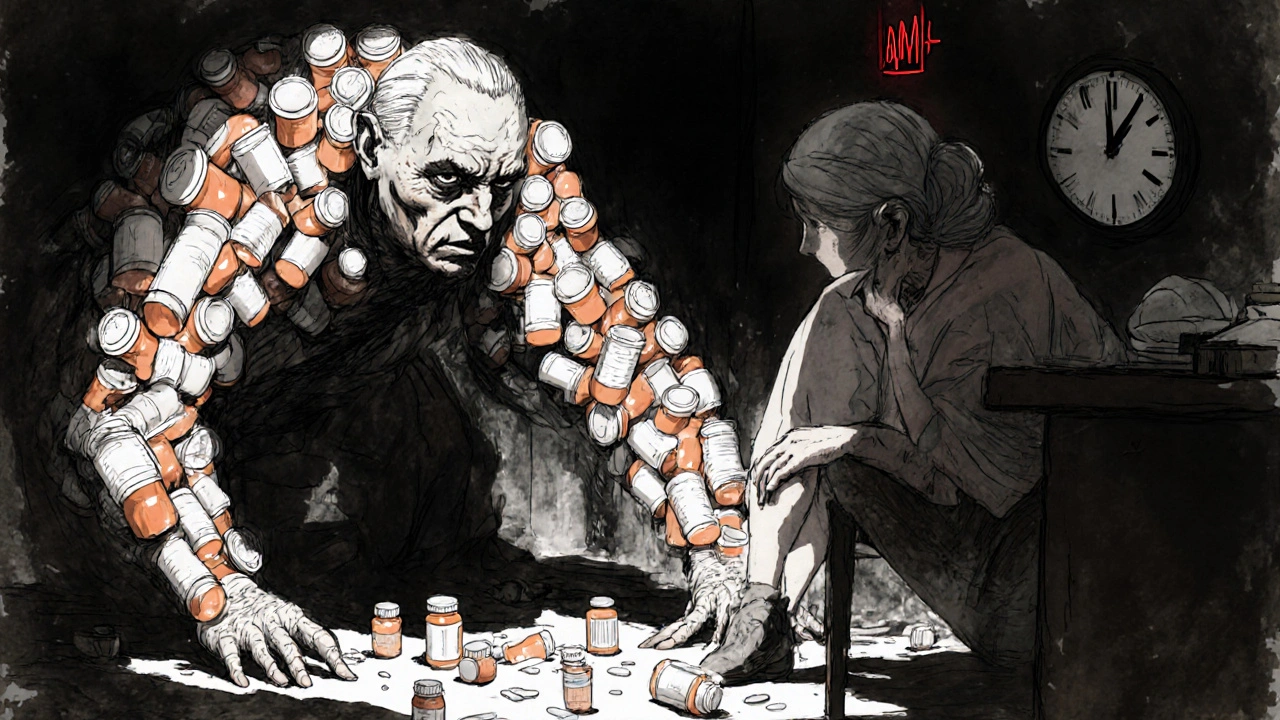
It’s easy to assume that if you’re taking a medication as prescribed, you’re safe. But the truth is, even common drugs can trigger life-threatening reactions-sometimes within hours. You might not realize you’re in danger until it’s too late. That’s why knowing the red flags for medication emergencies isn’t just helpful-it could save your life.
What Counts as a Medication Emergency?
Not every side effect needs an ambulance. Nausea after antibiotics? That’s common. But if you start vomiting nonstop, can’t keep fluids down, and feel dizzy? That’s dehydration-and it’s dangerous. The line between a bothersome side effect and a medical emergency comes down to severity, speed, and system-wide symptoms.The U.S. Food and Drug Administration defines serious adverse drug reactions as those that cause death, hospitalization, disability, or permanent damage. About 106,000 people die each year in the U.S. from these reactions. Most aren’t from overdoses-they’re from drugs taken exactly as directed.
Top Red Flags That Demand Immediate Help
Some symptoms are unmistakable. If you experience any of these after starting a new medication or changing a dose, call 999 or go to the nearest emergency department right away:
- Difficulty breathing or wheezing-even if it feels like an asthma flare-up, it could be anaphylaxis.
- Swelling of the lips, tongue, or throat-this can block your airway within minutes.
- Blue or gray lips or fingernails-this means your body isn’t getting enough oxygen.
- Sudden, severe rash with blistering or peeling skin-this could be Stevens-Johnson Syndrome, a rare but deadly reaction often triggered by antibiotics or painkillers.
- Chest pain, rapid or irregular heartbeat-especially if you’re on blood thinners, antidepressants, or heart medications.
- Slurred speech, weakness on one side of the body, or sudden confusion-these mimic stroke and can be caused by drug interactions affecting blood pressure or clotting.
- Blood pressure above 180/120 mmHg with headache, vision changes, or nausea-this is a hypertensive emergency.
- Temperature above 102°F with chills and confusion-could signal a dangerous reaction like drug-induced fever or sepsis.
- Unexplained bleeding-nosebleeds that won’t stop, blood in urine or stool, bruising without injury-especially if you’re on warfarin, aspirin, or newer anticoagulants like apixaban.
Common Culprits and Their Hidden Risks
Some medications are more likely to cause emergencies than others. Penicillin and sulfa drugs top the list for severe allergic reactions. But other everyday drugs carry hidden dangers:
- Antibiotics like amoxicillin or ciprofloxacin-can trigger anaphylaxis or dangerously raise INR levels when taken with warfarin, increasing bleeding risk by up to 50%.
- NSAIDs like ibuprofen or naproxen-combine with blood thinners and can cause internal bleeding, even in people who’ve taken them for years without issue.
- Insulin or diabetes drugs-can cause dangerously low blood sugar leading to seizures or coma if not treated fast.
- St. John’s Wort and other herbal supplements-many people don’t realize these interact with antidepressants, birth control, and heart meds. One study showed 30% of patients on multiple medications didn’t tell their doctor about supplements they were taking.
- Barbiturates and seizure medications-can cause skin reactions like TEN, which kills 30-50% of patients if not treated immediately.
It’s not just about the drug itself-it’s about combinations. Over 15,000 drug interactions are documented. About 700 of them are serious enough to cause death. If you’re taking three or more medications daily, your risk doubles. If you’re on five or more, your risk triples.

When It’s Not an Emergency (But Still Needs Attention)
Not every strange feeling means you’re dying. Mild rashes without breathing trouble? That’s usually not anaphylaxis. A little nausea with antibiotics? Common. But here’s the catch: if those symptoms get worse, or new ones appear, you need to act.
For example:
- A mild rash that spreads over 24 hours? Call your pharmacist or GP.
- Headache after starting a new blood pressure med? Wait 24 hours. If it’s still there or gets worse, get checked.
- Constipation with opioids? That’s expected-but if you haven’t had a bowel movement in 4 days and feel bloated or nauseous, you could be developing a bowel obstruction.
Timing matters. Sixty-eight percent of severe reactions happen within 72 hours of starting a new drug or changing the dose. That’s why you should monitor yourself closely during that window.
Why People Wait Too Long
Most patients don’t know what to look for. A 2023 Mayo Clinic survey found 61% of people weren’t sure whether their symptoms required emergency care. Only 42% received clear instructions from their doctor or pharmacist about when to seek help.
Stories from patient forums tell the same tale. One Reddit user started amoxicillin and developed a rash and swelling-but waited four hours, thinking it was "just an itch." By the time they went to the hospital, their throat was closing. Another person took ibuprofen for back pain and didn’t realize the black, tarry stool meant internal bleeding.
Doctors and pharmacists aren’t always better at spotting these either. A third of anaphylaxis cases are misdiagnosed as asthma or panic attacks. That’s why you can’t rely on someone else to recognize the danger-you need to know the signs yourself.
What You Can Do Before It Happens
Prevention starts before you even take the pill:
- Make a full list of everything you take-prescription drugs, over-the-counter meds, vitamins, and herbal supplements. Bring it to every appointment.
- Ask your pharmacist: "What are the red flags for this medication? What should I watch for in the first few days?" They’re trained to catch these risks.
- Know your baseline. If you’re on blood thinners, know your normal INR range. If you have high blood pressure, know your usual readings.
- Set phone alerts for the first 72 hours after starting a new drug. Check in with yourself: "Any new symptoms? Any change in breathing, skin, or energy?"
- Keep an epinephrine auto-injector if you have a known severe allergy. Use it immediately if you feel throat swelling or trouble breathing-then call 999. Don’t wait to see if it gets better.
The Bigger Picture
The U.S. spends billions each year treating preventable medication emergencies. New systems like the FDA’s Sentinel Initiative now monitor hundreds of millions of patient records to catch dangerous patterns faster. Pharmacist-led medication reviews are now covered by Medicare for high-risk patients-and they’ve cut emergency visits by 18%.
But technology won’t help if you don’t know what to look for. The most dangerous reactions are the ones that look like something else-a stroke, a heart attack, an infection. That’s why your awareness is the last line of defense.
Can a medication reaction happen days after I start taking it?
Yes. While 68% of severe reactions happen within 72 hours of starting a new drug or changing the dose, some reactions-like Stevens-Johnson Syndrome or drug-induced liver injury-can take days or even weeks to appear. If you develop a new rash, yellowing skin, dark urine, or unexplained fatigue more than a few days after starting a medication, get it checked.
Is it safe to wait and see if a mild side effect goes away?
It depends. Mild nausea, dizziness, or dry mouth often fade as your body adjusts. But if symptoms get worse, spread, or are joined by new ones-like swelling, trouble breathing, or confusion-don’t wait. Track the timeline: if a symptom lasts more than 48 hours or interferes with eating, sleeping, or moving, contact your pharmacist or doctor. Better safe than sorry.
Can over-the-counter drugs cause emergencies?
Absolutely. Common OTC drugs like ibuprofen, naproxen, and even high-dose acetaminophen can cause serious reactions. Ibuprofen can trigger bleeding when mixed with blood thinners. Acetaminophen overdose is the leading cause of acute liver failure in the U.S. Even antihistamines like diphenhydramine can cause confusion, urinary retention, or dangerous heart rhythms in older adults.
What should I do if I think I’m having a reaction but I’m not sure?
Call 111 or your pharmacist first. They can help you assess whether it’s urgent. If you’re unsure and have any of the red flag symptoms-trouble breathing, swelling, chest pain, slurred speech, or sudden weakness-go to the emergency department. Don’t wait for someone else to tell you it’s serious. Your instincts matter.
Are older adults at higher risk for medication emergencies?
Yes. Nearly half of Americans over 65 take five or more medications daily. Their bodies process drugs slower, and they’re more likely to have multiple health conditions that interact. They’re also more prone to side effects like dizziness (which can lead to falls) and confusion. Always ask for a medication review if you or a loved one is on multiple prescriptions.
How do I report a bad reaction to a medication?
Report it to the Yellow Card Scheme in the UK, or the FDA’s MedWatch program in the U.S. Even if you’re not sure it was the drug, report it. These reports help regulators spot dangerous patterns. Your report could prevent someone else from having the same reaction.
Final Thought: Your Body Knows Before You Do
Medications are powerful. They fix problems-but they can also create them. The difference between a bad day and a life-threatening event often comes down to one thing: whether you recognize the warning signs early.
Don’t second-guess yourself. If something feels wrong after starting a new drug, trust that feeling. Write down your symptoms. Call your pharmacist. Go to the hospital if needed. You don’t need to be an expert to save your own life-you just need to know what to look for.

Kihya Beitz
November 15, 2025 AT 22:13So let me get this straight - if I take a pill and my lips turn blue, I’m supposed to panic? Cool. Meanwhile, my doctor didn’t even ask if I was on St. John’s Wort. Guess I’ll just add that to my list of things I’m not telling my healthcare providers because why not? 🤷♀️
Jennifer Walton
November 17, 2025 AT 14:58Medication isn’t magic. It’s chemistry. And chemistry doesn’t care about your intentions.
BABA SABKA
November 19, 2025 AT 04:32Let’s be real - this is systemic negligence. Pharma’s profit model thrives on polypharmacy. You got 5+ meds? Congrats, you’re a walking pharmacokinetic experiment. The FDA doesn’t regulate interactions - they just collect reports after the fact. This isn’t healthcare. It’s pharmacological Russian roulette with a 70% chance of misdiagnosis. And don’t even get me started on OTC drugs being sold like candy.
Chris Bryan
November 20, 2025 AT 08:23They’re hiding the truth. The CDC knows 80% of these reactions are caused by government-mandated formularies. Why else would they push so many combo pills? And why do all the red flags sound exactly like symptoms of 5G-induced neurotoxicity? Someone’s controlling the narrative. Check your INR - it’s probably being manipulated remotely.
Jonathan Dobey
November 21, 2025 AT 07:17Ah, the beautiful tragedy of modern pharmacology - a paradox wrapped in a capsule, dipped in corporate greed, and labeled ‘essential.’ We’ve turned the human body into a symphony of chemical dissonance, where every pill is a note in a composition no one composed - and no one can conduct. The real emergency? Not the reaction. The fact that we’ve outsourced our biological sovereignty to a system that profits from our ignorance. You think Stevens-Johnson Syndrome is caused by amoxicillin? No. It’s caused by the illusion that safety can be prescribed.
ASHISH TURAN
November 22, 2025 AT 00:39I’ve been on 6 medications for 3 years now. My pharmacist sat with me for 45 minutes and mapped every interaction. I didn’t know St. John’s Wort could mess with my birth control - now I don’t take it. Small steps. Knowledge is power, not fear.
Ryan Airey
November 23, 2025 AT 19:57Everyone’s just too lazy to read the damn leaflet. You want to live? Learn your meds. Don’t just trust the ‘take once daily’ sticker. Look up the interactions. Know your baseline. If you can’t be bothered, don’t complain when your kidneys fail. This isn’t rocket science - it’s basic responsibility.
Hollis Hollywood
November 25, 2025 AT 16:22I’ve seen so many people dismiss early symptoms because they didn’t want to be a bother. I had a friend who ignored the rash after starting a new antibiotic - thought it was just ‘heat.’ By the time she got to the ER, she was in multi-organ failure. It took six weeks in the hospital. She’s fine now, but she’ll never forget it. I just wish more people knew that ‘it’s probably nothing’ is the most dangerous phrase in medicine. Your body doesn’t lie - it just whispers until you scream.
Aidan McCord-Amasis
November 27, 2025 AT 08:09Bro, I took ibuprofen and got a rash. Thought it was just stress. Then I Googled it. Holy shit. Went to urgent care. Turned out it was early SJS. 🚨 They saved me. Don’t be me. 🙏
Adam Dille
November 28, 2025 AT 13:14My grandma takes 8 pills a day. I made her a little chart with color-coded alerts for red flags. We check in every morning. She says it’s the first time she’s felt safe with her meds. Small wins, y’all. 💙
Katie Baker
November 28, 2025 AT 20:44This post saved my life. I started a new blood pressure med and got a weird headache. I almost brushed it off - but then I read this. Called my pharmacist. Turns out it was a dangerous interaction with my supplement. We adjusted everything. I’m alive because I listened. Thank you.